The group traumatic episode protocol (G-TEP): A service evaluation of a single session group intervention for healthcare staff in the acute adolescent inpatient setting
This paper evaluates a single-session group intervention that has been implemented to reduce trauma-based symptoms and levels of distress for healthcare professionals working on (and associated with) acute adolescent psychiatric wards. This group was based on the eye movement desensitisation and reprocessing (EMDR) therapeutic model and followed Shapiro’s already established group protocol; EMDR group traumatic episode protocol (G-TEP). Results from this early EMDR intervention (EEI) demonstrated a large effect size indicating a significant reduction in trauma-based symptoms between pre-intervention and at one-month follow-up (n=21) (Cohen’s d = 1.4). Comparisons showed that on average, trauma-based symptoms had reduced to below clinical concern thresholds by follow-up. A downward trend was also observed in distress levels throughout the intervention. Feedback showed that 81.8% of participants felt that the session had been useful, and 78.8% felt able to implement learnings from the session in their work or home life.Staff seemed to receive G-TEP favourably and find it effective. Compassionate leadership and the potential benefits of attending responsively to staff well-being issues are also outlined.
Introduction
Healthcare professionals are considered to be at a higher risk of developing post-traumatic stress disorder (PTSD) due to workplace violence and other traumatic events at work (Carleton et al., 2019; Stelnicki et al., 2020). Eye movement desensitisation and reprocessing (EMDR) is a psychotherapy approach informed by the adaptive information processing model. The model suggests that new and highly stressful experiences can overwhelm an individual’s nervous system, impairing memory processing and leaving the experience stored in a dysfunctional and unprocessed form. This may lead to higher levels of distress and the development of trauma-based symptoms (Shapiro, 2007; Kaptan et al., 2020). Unlike other psychosocial therapies, EMDR uses techniques known as bilateral stimulation (BLS) which typically involve guiding clients through sets of rapid eye movements, tapping or auditory BLS, while focusing on the traumatic memory and its associated thoughts and feelings (Lee & Cuijpers, 2013).
EMDR has been found to be effective in reducing symptoms of PTSD (Khan et al., 2018), depression (Wood & Ricketts, 2013) anxiety (Yunitri et al., 2020), distress from chronic pain (Tesarz et al., 2014) and medically unexplained symptoms (Van Rood & De Roos, 2009); as well as showing promising results across different ages (Ahmad et al., 2007), and in non-clinical (Ter Heide et al., 2016; Aduriz et al., 2009) and clinical settings (Chen et al.,2015). The World Health Organization (WHO, 2013) National Institute for Health and Care Excellence (NICE, 2018) and International Society for Traumatic Stress Studies (ISTSS, 2018) all recommend EMDR as a treatment for PTSD. Recently, a multi-agency study has shown that EMDR therapy is more cost-effective than other trauma- focused treatments due to its brief and structured 8-phase protocol (Mavranezouli et al., 2020).
While EMDR has mostly been evaluated as a one-to-one intervention, this type of delivery may not be the most cost or time-effective approach for the rising number of mental health difficulties (Gil-Rivas et al., 2019), particularly considering the detrimental impact of the recent COVID-19 pandemic on mental health (Xiong et al., 2020). An EMDR group intervention might represent a more efficient alternative for delivering this effective treatment to many. There have been several group protocols developed in line with the EMDR model, one of them being the EMDR Group Traumatic Episode Protocol (G-TEP) (Shapiro, 2013). It has been designed as a group alternative of the evidence-based Recent Traumatic Episode Protocol (R-TEP) (Shapiro & Laub, 2014) which focuses on recent traumatic or distressing memories and works on desensitisation, rather than complete reprocessing. The G-TEP protocol incorporates the eight phases of the original EMDR protocol and attempts to keep the power of individual EMDR while making it accessible in a group setting (Lehnung et al., 2017). It can be applied to recent traumatic events and follows a uniquely developed worksheet focusing on simple stabilisation and containment exercises (Shapiro, 2007; 2012). The protocol starts with a safety screening exercise to identify those not sufficiently prepared for group trauma processing. The G-TEP intervention is a highly structured procedure that follows a therapist manual closely, which makes it ideal for focusing solely on recent and ongoing points of disturbance (PODs)/distress. The underlying mechanism is focused on ring-fencing the distress within a timeframe (onset to present day) to enable desensitisation (and possible processing) of trauma.
A recent systematic review has shown that EMDR group protocols are effective in significantly reducing PTSD, depression and anxiety symptoms and have several advantages compared to the individual intervention, including reducing waiting lists considerably, offering group support and using other means of expressing trauma rather than just through talking therapy (Kaptan, et al., 2021). However, the review also highlighted intrinsic difficulties with group work such as the inability to verbalise distressing memories and accommodating for the varying individual needs within a group.
In the current service evaluation project, the EMDR G-TEP intervention was delivered via a single-session primarily to mental health staff in an acute, adolescent, psychiatric inpatient service (consisting of two wards caring for 13–18-year-old patients). Across the service there has been a rise in chronicity and severity of cases admitted. Incidents of violence towards staff have also increased. This has led to higher distress levels among staff, which may impact the therapeutic relationships between the young person and their treating team. Consequently, compassion fatigue, traumatic stress, vicarious trauma, and burnout have come to be seen as occupational hazards for professionals working in these specialised contexts (Bhagwagar, 2022; Figley, 2002).
This account from our service is supported by the literature. Healthcare professionals are considered to be at higher risk of developing PTSD and other mental health difficulties such as depression, anxiety, burnout, and psychological distress due to exposure to workplace violence and other traumatic events at work (Carleton et al., 2019; Stelnicki et al., 2020; Mento, et al., 2020; Seto et al., 2020; Rudkjoebing et al., 2020). Workplace violence is especially prevalent in psychiatric and mental health settings (Liu et al., 2019; Mento et al., 2020). It has been found that along with traumatic events, workplace chronic stressors and burnout are associated with PTSD among psychiatric and mental health professionals (Hilton et al., 2020), and burnout specifically may mediate the association between traumatic events and PTSD symptoms (Ham et al., 2022).
Workplace stressors have also been linked with decreased productivity, increased staff absence and turnover, and reduced quality of patient care (Liu et al., 2019; Mento et al., 2020). This serves to highlight the need for a therapeutic intervention for staff that focuses on reducing and managing trauma-based symptoms, and the consequent risk of burnout following critical, traumatic events in psychiatric and healthcare settings.
In order to support staff with traumatic workplace incidents and trauma-based symptoms, a specific support group focusing on the established EMDR G-TEP protocol was set up within our acute, psychiatric inpatient service for adolescents. It is important to emphasise that this group intervention did not recruit individuals with a clinical presentation or a diagnosis of PTSD but focused on reducing stress and trauma-based symptoms experienced by any staff following recent traumatic workplace incidents. This delivery is supported by the EMDR model, as originally, EMDR was regarded as an intervention to improve trauma-based symptoms and address ‘experience-based’ psychological distress more generally rather than as a treatment for a specific mental health difficulty (Shapiro, 1989). Psychological outcomes were routinely collected by the service throughout the running of the group and are presented below.
Outcomes
The primary outcome measure was the effectiveness of the single-session support group intervention in reducing trauma-based symptoms of hypervigilance, avoidance and intrusions, and subjective levels of distress, in staff members who have experienced a traumatic or stressful event whilst at work. Secondary outcomes were how helpful and useful the participants found the intervention and observing the trend of the measured distress levels throughout the single-session intervention. Comparison of trauma-based symptoms with clinical thresholds from the evidence-base was also planned.
Methods
Ethical considerations
This service evaluation was approved by the service’s research and development team and by the Faculty of Medicine and Health Sciences Research Ethics Subcommittee from the University of East Anglia. All participants provided their written consent for their data to be used in this service evaluation. Prior to data being shared for analysis, data was anonymised and matched with an ID number to ensure confidentiality and full anonymity.
Design
This is a retrospective quantitative service evaluation considering within-group comparisons of routinely collected anonymous outcome data.
Participants
All staff working at the service were eligible to participate in this study. Participants could directly self-refer at any stage into the group by contacting the facilitators or could be referred following discussions in staff monthly management supervision with senior team members. Also, staff were followed up after serious incidents on the psychiatric wards and were offered the group intervention. Typically, recruitment occurred through word-of-mouth, flyers, reminders, recommendations from staff who attended previously, and supervision with senior team members.
Power calculation
Utilising G*Power software (Erdefelder et al., 1996), a power calculation (with power set at 0.8) was conducted to determine the minimum number of participants required to achieve a medium effect size (0.5) at a 0.05 significance level for a one-tailed project. The results indicated that a minimum of 28 participants were required for a non-parametric test, and 27 were required for parametric testing. In total 33 participants enrolled into the group, with 21 of these able to be matched across pre and follow-up outcome measures. Following this, a post-hoc power analysis was conducted to determine the achieved power given the effect size calculated from the data collected (d=1.4 indicating a very large effect size), alpha at 0.05 and the total sample size of matched participants (n=21). The achieved power calculated was found to be 0.99. Therefore, despite not reaching the required sample size initially determined, a post-hoc analysis computed that the study was adequately powered based on the effect size and sample size obtained.
Procedure
The single-session supportive group intervention was held face-to-face, once a month within the service, with a follow-up contact/consultation one month later. The intervention for up to six active participants, was a two-hour session focusing on stressful and traumatic workplace memories. Participants were able to be referred back to the group following completion through the same recruitment process. The intervention followed the G-TEP protocol and therapist manual closely. There were three facilitators in the session which included a psychotherapist who was an accredited consultant and clinical supervisor in EMDR with specific G-TEP training, alongside a clinical psychologist and an assistant psychologist who were trained internally to deliver the G-TEP protocol through modelling, self-study and supervision. Attendees could process different traumatic material and situations, as the mode of therapeutic change was internal processing rather than verbal dialogue. Also, participants were asked not to share any negative imagery/material within the group.
Basic demographic information including role type, contract type and ward affiliation was collected followed by completion of the revised Impact of Event Scale (IES-R) (Weiss & Marmar, 1996; Horowitz et al., 1979). An introduction, involving significant psychoeducation with respect to stress, trauma, and its effect on the brain was provided. The G-TEP protocol was followed and throughout the intervention, subjective units of distress (SUD) were taken at several time points across the two hours (see Outcome measures section for more details). Participants then completed the post-intervention feedback form immediately following the intervention. This whole process took two hours to complete.
Each participant was contacted one month after attending to evaluate the effectiveness of the intervention. The IES-R and the brief follow-up feedback form were completed. Participants were usually contacted via email, or in person on the ward, for the one-month follow-up. If there was no email reply, they were followed up at their next shift on the ward close to the follow-up date. Participants at follow-up who wanted further support, were signposted towards a range of options both internally and externally. Participants could also be re-referred back into the group.
Outcome measures
The measures outlined below were pre-determined and routinely collected by the service.
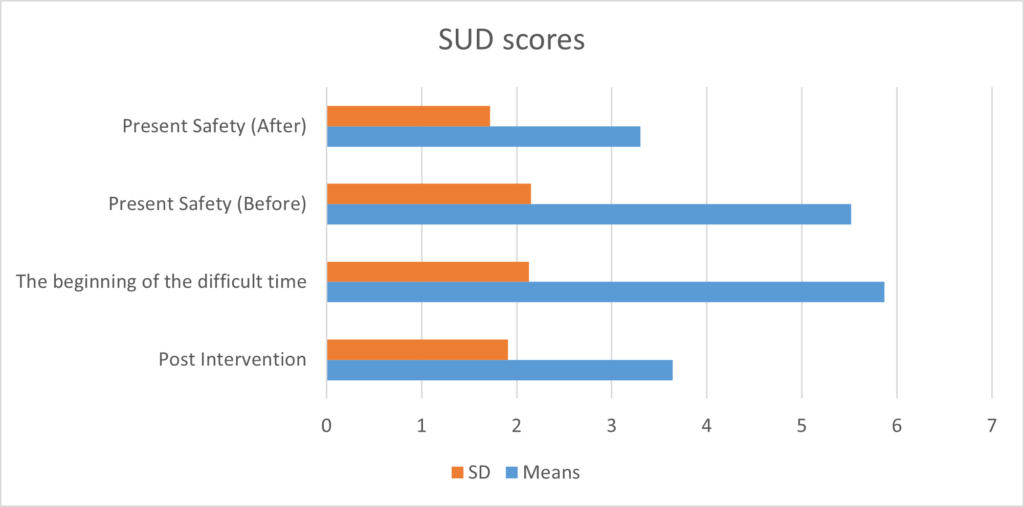
Subjective Units of Distress Scale
SUD ratings on 10-point scales for distress intensity were taken prior to the present-safety exercise and after the present-safety exercise. A separate SUD rating (labelled as ‘The beginning of the difficult time’) was made prior to starting the three focused desensitisation and processing exercises. SUD were measured at the start and end of all three points of disturbance (PoD) exercises as well as after the 3rd, 6th and 9th sets of BLS of each PoD. Participants further recorded an overall rating following the completion of all exercises. Utilising SUD is a commonly used method for measuring levels of distress experienced within intervention sessions and has been used frequently in research and clinical settings (Benjamin et al., 2010; Matheson, 2014; Wolpe, 1990).
Impact of Event Scale-Revised
A 22-item self-report measure that assesses subjective distress caused by a traumatic event. This measure was completed on the day of the intervention and at follow-up. As the IES-R enquires about symptoms experienced during the past seven days, the data collected on the day of the intervention was essentially a pre-intervention measure of symptoms. The total score ranges from 0-88 and subscale scores can also be calculated for intrusion, avoidance, and hypervigilance. These subscales correspond to trauma-related symptoms and have been shown to have good reliability, and separable constructs with the same amount of variance, indicating high stability. Also, the IES-R has a high convergent validity, particularly between intrusion, avoidance, and PTSD diagnosis in a number of studies. This validates its use as a helpful screening measure of stress reactions following a range of traumatic events (Sundin & Horowitz, 2002). In addition, it is a short self-report measure and therefore has a low-cost for detecting trauma symptoms (Rothbaum et al., 1992).
A 12-item study-derived mixed qualitative and quantitative feedback form
A uniquely designed feedback form including a Likert scale for some questions and open-ended questions to gather qualitative data. The feedback form included questions about how useful and helpful the session was, where it could be improved and whether participants would like further support. This questionnaire was completed at post-intervention and was used as there was no existing psychometric that captured this experience.
A 7-item follow-up feedback form
At one-month follow-up, participants were asked to complete a short feedback form. There was also another opportunity for participants to inform the team whether they would like any further support.
Analysis and results
The data from 33 participants who took part and completed the G-TEP intervention were included. Data was cleaned and incomplete data sets were removed and only those participants who completed both measures were used for purposes of statistical analysis (n=21). Statistical analysis was performed using SPSS Statistics software. Significance was considered when p<0.05. Demographic information for role, contract type and ward name were recorded for each participant, the majority of participants (57%) were nurses or healthcare assistants. All 33 participants completed the feedback questionnaire on the day of intervention, but only 21 completed both the pre and 1-month follow-up IES-R. This was because the IES-R was introduced after the group had already been run twice
Primary outcomes
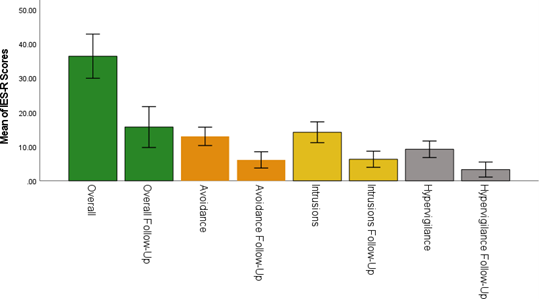
Outcomes from the IES-R were analysed using a repeated measure, paired t-test to evaluate the intervention. Means and standard deviations (SD) for the overall and subscale scores on the IES-R relating to pre-intervention and at follow-up were calculated (Figure 1).
Analysis showed a large significant difference, t(20)= 6.41, p-value < 0.001 (Cohen’s d =1.40) for total IES-R scores, with significantly lower scores at follow-up. Significance was also found between all three subscales of avoidance (t(20)=4.57, p<0.001), intrusions (t (20)=5.39, p<0.001) and hypervigilance (t(20)=6.43, p<0.001). There was one outlier identified, but this was kept in the dataset as it was calculated that it did not impact or skew the dataset (overall: t(19)=6.67; avoidance: t(19)=4.33; intrusions: t(19)=5.65; hypervigilance: t(19)=6.15, with p<0.001, alpha at 0.05).
Secondary outcomes
Comparisons were drawn between the means from the IES-R at pre-intervention and at follow-up to clinical thresholds from the evidence base and are discussed further. SUD scores were collected at several time points throughout the session and a downward trend in distress levels was observed as participants progressed through each exercise/PoD. It was not possible for participants to be matched across all intervals with only 69.58% of data being collected for all three PoDs, and consequently statistical analysis was not conducted for SUD scores. Means and SD were calculated for each timepoint (Figure 2).
Qualitative elements of the feedback questionnaires
The majority of participants (73%) felt less troubled/anxious about the incident than when they first came into the session and all of the participants agreed that they had learnt some practical strategies to help them cope with the difficult memory. A similarly large proportion (97%) felt that they could continue to use these strategies after the session and whilst they were at work and that they would recommend the intervention to others.
These positive trends were maintained at the one month follow up with the majority of people (76%) feeling less distress when thinking about the memory and 73% finding the memory less intrusive. The same number (73%) were using the coping strategies that had been taught in the sessions and just over half of the participants (51%) still felt anxious about coming in to work.
Overwhelmingly, participants felt that the G-TEP intervention had been useful (82%) and almost the same number (79%) have used things they learnt in other areas of their lives.
Discussion
This paper describes the service evaluation of an early intervention EMDR G-TEP group for healthcare staff working in an acute adolescent inpatient setting. This was in the local context of rising rates of traumatic incidents including violence towards healthcare professionals, and more widely with higher rates identified in psychiatric inpatient settings, and in research (Liu et al., 2019).
The results show a reduction in trauma symptoms following the single session G-TEP intervention. At the one-month follow-up this reduction was clinically and statistically significant, both in total scores and in individual subscale scores of the IES-R measure. The fact that 79% of participants continued to implement the EMDR-informed stabilisation strategies taught in the session, may account for some of this reduction. Implementing EMDR stabilisation strategies such as these has been shown to significantly reduce stress in medical staff, a group of professionals also susceptible to mental health difficulties (Behnammoghadam et al., 2019), and has been evidenced as a useful self-help tool in situations of increased stress (Aziraj-Smajic & De la Fosse, 2021). Specifically, findings by Yurtsever et al. (2018) and Lehnung et al. (2017) have demonstrated the effectiveness of EMDR G-TEP strategies in reducing PTSD and trauma-based symptoms.
These findings are in line with studies looking at a computerised adaptation of the EMDR G-TEP protocol which was effective in reducing symptoms of depression, anxiety and stress among mental health professionals following stressful workplace events (Moench & Billsten, 2021) and in preventing vicarious trauma in professionals working with child abuse (Tsouvelas et al., 2019). Tsouvelas et al. (2019) also found that the strategies learnt in the EMDR G-TEP extended beyond a specific traumatic event focused on in the session, as participants reported that emotional distress in the workplace had reduced, potentially suggesting a change in adaptive processing of traumatic and stressful events at work.
Early EMDR interventions such as G-TEP, have been identified as crucial to prevent burnout and mental exhaustion, lowering risk in developing mental health difficulties (Fiorillo & Gorwood, 2020), with single-session EMDR having promising evidence for efficacy (ISTSS, 2019). Hilton et al. (2021) highlighted that post-traumatic burnout, compassion fatigue, poor mental health and low compassion and satisfaction are key risk factors for PTSD, and interventions that support mental health professionals in their coping and wellbeing following traumatic events may be valuable in preventing PTSD among psychiatric nurses.
The data collected further showed that clinical thresholds for PTSD were exceeded at pre intervention with an average score of 36. This score had reduced to 15 by one-month follow- up. Research indicates that scores exceeding 24 are clinically concerning (Asukai et al., 2002), and scores exceeding 33 represent the best cut-off for a probable diagnosis of PTSD (Creamer et al., 2002). This suggests that healthcare staff in this study were experiencing trauma-based symptoms at levels concurrent with a PTSD diagnosis, which reduced to below clinical concern at follow-up. However, a survey among 761 psychiatric staff, showed 16% met thresholds for PTSD, with nursing staff scoring the highest (Hilton et al., 2020), therefore indicating a much lower rate than the population in our service evaluation. It can also be suggested that participants who opted to enroll into the G-TEP intervention found it especially difficult following a traumatic event, which may explain the elevated rate of trauma-based symptoms when compared with studies that capture the general population of healthcare workers. However, only data was available for staff who underwent the intervention (and were likely in need of doing so) and not for all staff working in this particular inpatient unit, which is likely to explain the high rate of trauma-based symptoms in comparison to studies that capture the general population of psychiatric inpatient healthcare workers (Hilton et al., 2020).
This service evaluation also gives rise to ethical issues around workers in psychiatric settings being given appropriate training on the potential impact of traumatic stress and coping techniques, as well as appropriate pathways for therapeutic support. In this study, there were clear pathways for support and many opportunities provided to request it. A combination of environmental changes to reduce traumatic incidents in healthcare settings (Hilton et al., 2020), appropriate training (Arbury et al., 2017), and access to staff wellbeing interventions/support focused on reducing stress and burnout (Ham et al., 2022) are all needed to reduce PTSD and trauma-based symptoms in healthcare workers. It is however important not to overlook workplace and organisational factors that may be associated with precipitating trauma-based symptoms such as workload, reward, fairness, and autonomy (Ham et al., 2022), as well as factors that may reduce the risk of symptoms and contribute to trauma recovery such as shared group experiences of similar traumatic events (Van de Ven, 2020; Eyre, 2022). Future research is required to look at longitudinal workplace factors such as these on psychiatric and healthcare staff to understand their associations with trauma-based symptoms and inform effective, therapeutic intervention targets.
This service evaluation provided a relatively small dataset, which reduces its generalisability to the wider healthcare population. However, the effect size (Cohen’s d = 1.4) indicated a very large effect for the intervention and it was clear that the EMDR G-TEP intervention reduced trauma-based symptoms in this population of psychiatric healthcare workers.
Final thoughts and clinical implications
In environments such as this, where patients are acutely unwell, and experiencing a radical change in environment and locus of control, incidents are likely to happen. This happens even when staff are trained to prevent and de-escalate incidents. Inpatient wards are high pressure and stressful environments where staff are confronted with serious and risk-laden situations on a frequent basis. The findings of our service evaluation indicate that when staff were allowed to participate in this two-hour, early EMDR-informed intervention, it was favourably received, and found to be effective. It seemed that having had a positive experience, participants were more likely to use the strategies learned to further help themselves, and to assist patients and others who experience stress/distress. Clearly this is a positive outcome for this type of environment, and beyond, given that many healthcare workers rotate regularly around wards and services. We hope that staff might repeat and recommend things which they find helpful.
For such an intervention to work in an inpatient setting it is essential that there is buy-in from managers and human resources, as well as ward/unit managers who need to work proactively at freeing up staff to attend such initiatives. There are many benefits from attending G-TEP such as learning about trauma, reducing anxiety about attending work, developing the ability to self-regulate and co-regulate, as well as reducing trauma symptoms. There is a case to be made for staff rotating into the intervention regularly so as to prevent the accumulation of stressful events. This can also help staff think about what they can do for themselves, their colleagues, and patients, in the immediate aftermath of situations and incidents. Staff well-being initiatives are increasingly being recognised as an essential part of compassionate leadership and may contribute to the retention and well-being of staff doing very challenging work in difficult circumstances.
In this type of setting, and probably many other similar settings, G-TEP appears to be an effective and responsive way of attending to staff well-being, by desensitising stressful and distressing work-based events. Such incidents ought not to be accepted as just part and parcel of the job. Services have a moral responsibility and duty to ensure that work-based psychological (and physical) wounds are fully attended to. The benefit of attending to staff wellbeing is not just for the staff themselves, but also for the quality and effectiveness of patient care too.
Acknowledgements
The authors would like to thank the staff members of the St Aubyn Centre who took part in this intervention and consented to their information being evaluated. Thanks also go to: Dr Jennifer Scott, Leah Simmons and Chong-Yui Chan for their co-facilitation of the groups, and data collection.
References
Adúriz, M. E., Bluthgen, C., & Knopfler, C. (2009). Helping child flood victims using group EMDR intervention in Argentina: Treatment outcome and gender differences. International Journal of Stress Management, 16 (2), 138–153. doi:10.1037/a0014719
Ahmad, A., Larsson, B., & Sundelin-Wahlsten, V. (2007). EMDR treatment for children with PTSD: Results of a randomized controlled trial. Nordic Journal of Psychiatry, 61(5), 349–354. doi:10.1080/ 08039480701643464
American Psychological Association. (2013). Publication manual of the American Psychological Association (6th edition). Washington DC: American Psychological Association Press.
Arbury, S., Zankowski, D., Lipscomb, J., & Hodgson, M. (2017). Workplace violence training programs for health care workers: An analysis of program elements. Workplace Health & Safety, 65(6), 273. doi:10.1177/2165079917712524
Asukai, N., Kato, H., Kawamura, N., Kim, Y., Yamamoto, K., Kishimoto, J., . . . Nishizono-Maher, A. (2002). Reliability and validity of the Japanese-language version of the Impact of Event Scale-Revised (IES-R-J): Four studies of different traumatic events. The Journal of Nervous and Mental Disease, 190(3), 175-182. doi:10.1097/00005053-200203000-00006
Aziraj-Smajiü, V., & De la Fosse, C. (2021). EMDR techniques and behavioural therapy in group training: Dealing with stress. Psychiatria Danubina, 33(1), 24-28.
Behnammoghadam, M., Kheramine, S., Zoladl, M., Cooper, R., & Shahini, S. (2019). Effect of eye movement desensitization and reprocessing (EMDR) on severity of stress in emergency medical technicians. Psychology Research and Behavior Management, 12, 289-296. doi:10.2147/prbm.s190428
Benjamin, C., O’Neil, K., Crawley, S., Beidas, R., Coles, M., & Kendall, P. (2010). Patterns and predictors of subjective units of distress in anxious youth. Behavioural and Cognitive Psychotherapy, 38(4), 497-504. doi:10.1017/s1352465810000287
Bhagwagar, H. (2022). Secondary trauma, burnout and resilience among mental health professionals from India: A review of research. Asian Journal Of Psychiatry, 76, 103227. doi:10.1016/j.ajp.2022.103227
Carleton, R., Afifi, T., Taillieu, T., Turner, S., Krakauer, R., Anderson, G., . . . McCreary, D. R. (2019). Exposures to potentially traumatic events among public safety personnel in Canada. Canadian Journal of Behavioural Science / Revue Canadienne Des Sciences Du Comportement, 51(1), 37-52. doi:10.1037/cbs0000115
Carleton, R., Afifi, T., Turner, S., Taillieu, T., Duranceau, S., LeBouthillier, D., . . . Asmundson, G. J. G. (2017). Mental disorder symptoms among public safety personnel in Canada. The Canadian Journal of Psychiatry, 63(1), 54-64. doi:10.1177/0706743717723825
Chen, L., Zhang, G., Hu, M., & Liang, X. (2015). Eye movement desensitization and reprocessing versus cognitive-behavioral therapy for adult posttraumatic stress disorder. Journal of Nervous & Mental Disease, 203(6), 443-451. doi:10.1097/nmd.0000000000000306
Creamer, M., Bell, R., & Failla, S. (2003). Psychometric properties of the Impact of Event Scale— Revised. Behaviour Research and Therapy, 41(12), 1489-1496. doi:10.1016/j.brat.2003.07.010
Erdfelder, E., Faul, F., & Buchner, A. (1996). GPOWER: A general power analysis program. Behavior Research Methods, Instruments & Computers, 28(1), 1–11. doi:10.3758/BF03203630
European Union. (2017). General Data Protection Regulation. http://eur-lex.europa.eu/legal- content/EN/TXT/PDF/?uri=CELEX:32016R0679&from=EN
Eyre, A. (2022). The Manchester attack support group programme: Modelling a psychosocial response to collective trauma. Journal of Psychosocial Studies, 15(1), 16-35. doi:10.1332/147867321×16490836655053
Figley, C. R. (Ed.). (2002). Treating compassion fatigue. New York: Brunner-Routledge.
Fiorillo, A., & Gorwood, P. (2020). The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. European Psychiatry, 63(1). doi:10.1192/j.eurpsy.2020.35
Gil-Rivas, V., Handrup, C. T., Tanner, E., & Walker, D. K. (2019). Global mental health: A call to action.
American Journal of Orthopsychiatry, 89 (4), 420–425. doi:10.1037/ort0000373
Ham, E., Seto, M., Rodrigues, N., & Hilton, N. (2022). Workplace stressors and PTSD among psychiatric workers: The mediating role of burnout. International Journal of Mental Health Nursing. doi:10.1111/inm.13015
Hilton, N., Addison, S., Ham, E., C. Rodrigues, N., & Seto, M. (2021). Workplace violence and risk factors for PTSD among psychiatric nurses: Systematic review and directions for future research and practice. Journal of Psychiatric and Mental Health Nursing, 29(2), 186-203. doi:10.1111/jpm.12781
Hilton, N., Ham, E., Rodrigues, N., Kirsh, B., Chapovalov, O., & Seto, M. (2020). Contribution of critical events and chronic stressors to PTSD symptoms among psychiatric workers. Psychiatric Services, 71(3), 221-227. doi:10.1176/appi.ps.201900226
Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of Event Scale: A measure of subjective stress. Psychosomatic medicine, 41(3), 209-218.
ISTSS. (2018). Posttraumatic stress disorder prevention and treatment guidelines methodology and recommendations. 1–29. Retrieved from http://www.istss.org/getattachment/Treating-Trauma/New-ISTSSPrevention-and-Treatment- Guidelines/ISTSS_ PreventionTreatmentGuidelines_FNL.pdf.aspx
Kaptan, S., Dursun, B., Knowles, M., Husain, N., & Varese, F. (2021). Group eye movement desensitization and reprocessing interventions in adults and children: A systematic review of randomized and nonrandomized trials. Clinical Psychology and Psychotherapy. doi:10.1002/cpp.2549
Khan, A. M., Dar, S., Ahmed, R., Bachu, R., Adnan, M., & Kotapati, V. P. (2018). Cognitive behavioral therapy versus eye movement desensitization and reprocessing in patients with post-traumatic stress disorder: Systematic review and meta-analysis of randomized clinical trials. Cureus. doi:10.7759/cureus.3250
Lee, C., & Cuijpers, P. (2013). A meta-analysis of the contribution of eye movements in processing emotional memories. Journal of Behavior Therapy and Experimental Psychiatry, 44(2), 231-239.doi:10.1016/j.jbtep.2012.11.001
Lehnung, M., Shapiro, E., Schreiber, M., & Hofmann, A. (2017). Evaluating the EMDR group traumatic episode protocol with refugees: A field study. Journal of EMDR Practice and Research, 11(3), 129-138.doi:10.1891/1933-3196.11.3.129
Liu, J., Gan, Y., Jiang, H., Li, L., Dwyer, R., Lu, K., . . . Lu, Z. (2019). Prevalence of workplace violence against healthcare workers: A systematic review and meta-analysis. Occupational and Environmental Medicine,76(12), 927– 937.
Matheson L. (2014). Your faithful brain: Designed for so much more! Nashville: WestBow Press.
Mavranezouli, I., Megnin-Viggars, O., Grey, N., Bhutani, G., Leach, J., Daly, C., . . . Pilling, S. (2020). Cost- effectiveness of psychological treatments for post-traumatic stress disorder in adults. PLOS ONE, 15(4), e0232245. doi:10.1371/journal.pone.0232245
Mento, C., Silvestri, M. C., Bruno, A., Muscatello, M. R. A., Cedro, C., Pandolfo, G., & Zoccali, R. A. (2020).Workplace violence against healthcare professionals: A systematic review. Aggression and Violent Behavior, 51, 101381
Moench, J., & Billsten, O. (2022). Randomized controlled trial: Self-care traumatic episode protocol, computerized EMDR treatment of COVID-19-related stress.
National Institute for Health and Care Excellence. (2018). Post-traumatic stress disorder: NICE guideline. Retrieved from www.nice.org.uk/guidance/ng116
Rothbaum, B. O., Ninan, P. T., & Thomas, L. (1996) Sertraline in the treatment of rape victims with post-traumatic stress disorder. Journal of Traumatic Stress, 9, 865–871.
Rudkjoebing, L., Bungum, A., Flachs, E., Eller, N., Borritz, M., & Aust, B., . . . Bonde, J. P. (2020). Work-related exposure to violence or threats and risk of mental disorders and symptoms: A systematic review and meta-analysis. Scandinavian Journal of Work, Environment and Health, 46(4), 339-349. doi: 10.5271/sjweh.3877
Seto, M., Rodrigues, N., Ham, E., Kirsh, B., & Hilton, N. (2020). Post-traumatic stress disorder, depression, anxiety symptoms and help seeking in psychiatric staff. The Canadian Journal of Psychiatry, 65(8), 577-583. doi:10.1177/0706743720916356
Shapiro, E., & Laub, B. (2014). The recent traumatic episode protocol (R-TEP): An integrative protocol for early EMDR intervention (EEI). In M. Luber (Ed.) Implementing EMDR early mental health interventions for man-made and natural disasters (pp. 193-215). New York: Springer Publishing.
Shapiro, E. (2007). 4 Elements exercise. Journal of EMDR Practice and Research, 1(2), 113–115.
Shapiro, E. (2012). EMDR and early psychological intervention following trauma. European Review of Applied Psychology, 62(4), 241–251.
Shapiro, E. (2013). The group traumatic episode protocol (G-TEP) for early EMDR intervention (EEI), Paper presented to the EMDR Turkey Symposium, Istanbul, Turkey.
Shapiro, F. (1989). Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories. Journal of Traumatic Stress, 2, 199–223. doi:10.1007/BF00974159
Shapiro, F. (2007). EMDR, adaptive information processing, and case conceptualization. Journal of EMDR Practice and Research, 1(2), 68-87. doi:10.1891/1933-3196.1.2.68
Stelnicki, A. M., Jamshidi, L., Angehrn, A., Hadjistavropoulos, H. D., & Carleton, R. N. (2020). Associations between burnout and mental disorder symptoms among nurses in Canada. Canadian Journal of Nursing Research,53(3), 254–263
Stelnicki, A., & Carleton, R. (2020). Mental disorder symptoms among nurses in Canada. Canadian Journal of Nursing Research, 53(3), 264-276. doi:10.1177/0844562120961894
Sundin, E., & Horowitz, M. (2002). Impact of Event Scale: Psychometric properties. British Journal of Psychiatry, 180(3), 205-209.doi:10.1192/bjp.180.3.205
Ter Heide, F., Mooren, T., Van de Schoot, R., De Jongh, A., & Kleber, R. (2016). Eye movement desensitisation and reprocessing therapy versus stabilisation as usual for refugees: Randomised controlled trial. British Journal of Psychiatry, 209(4), 311-318. doi:10.1192/bjp.bp.115.167775
Tesarz, J., Leisner, S., Gerhardt, A., Janke, S., Seidler, G. H., Eich, W., & Hartmann, M. (2014). Effects of eye movement desensitization and reprocessing (EMDR) treatment in chronic pain patients:
A systematic review. Pain Medicine (United States), 15(2), 247–263. doi:10.1111/pme.12303
Tsouvelas, G., Chondrokouki, M., Nikolaidis, G., & Shapiro, E. (2019). A vicarious trauma preventive approach. The group traumatic episode protocol EMDR and workplace affect in professionals who work with child abuse and neglect. Dialogues in Clinical Neuroscience and Mental Health, 2(3), 130-138.
Van de Ven, P. (2020). The journey of sensemaking and identity construction in the aftermath of trauma: Peer support as a vehicle for co-construction. Journal of Community Psychology, 48(6), 1825-1839. doi:10.1002/jcop.22373
Van Rood, Y., & De Roos, C. (2009). EMDR in the treatment of medically unexplained symptoms: A systematic review. Journal of EMDR Practice and Research, 3(4), 248-263. doi:10.1891/1933-3196.3.4.248
Weiss, D. S., & Marmar, C. R. (1996). The Impact of Event Scale – Revised. In J. Wilson & T. M. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399-411). New York: Guilford.
Wolpe, J. (1990). The practice of behavior therapy (4th ed.). Oxford: Pergamon Press.
Wood, E., & Ricketts, T. (2013). Is EMDR an evidenced-based treatment for depression? A review of the literature. Journal of EMDR Practice and Research, 7(4), 225–236. doi:10.1891/1933-3196.7. 4.225
World Health Organisation (2013). Guidelines for the management of conditions specifically related to stress. Assessment and management of conditions specifically related to stress. Retrieved from: https://apps.who.int/iris/bitstream/handle/10665/85119/9789241505406_eng.pdf;jsessionid= 5F6A190036078878726F29FDEB20115E?sequence=1
Xiong, J., Lipsitz, O., Nasri, F., Lui, L., Gill, H., Phan, L., . . . McCintyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55-64. doi:10.1016/j.jad.2020.08.001
Yunitri, N., Kao, C., Chu, H., Voss, J., Chiu, H., Liu, D., . . . Chou, K-R. (2020). The effectiveness of eye movement desensitization and reprocessing toward anxiety disorder: A meta-analysis of randomized controlled trials. Journal of Psychiatric Research, 123, 102-113. doi:10.1016/j.jpsychires.2020.01.005
Yurtsever, A., Konuk, E., Akyüz, T., Zat, Z., Tükel, F., Çetinkaya, M., . . . Shapiro, E. (2018). An eye movement desensitization and reprocessing (EMDR) group intervention for Syrian refugees with post- traumatic stress symptoms: Results of a randomized controlled trial. Frontiers in Psychology, 9. doi:10.3389/fpsyg.2018.00493



