Adapting a Trauma Pathway within an Improving Access to Psychological Therapy (IAPT) Service in the context of Increased Demand and severe acute respiratory syndrome coronavirus 2 (COVID-19)
Abstract
The 2018 National Institute for Health and Care Excellence (NICE) guidelines reference Eye Movement Desensitization and Reprocessing (EMDR) for consideration as an early intervention for trauma. EMDR is offered within Talking Helps Newcastle (THN), an IAPT service in the North East of England. However, due to rising demands on the service, it has been increasingly difficult to offer this recommended therapy in the timescale required for early intervention. The Group Traumatic Episode Protocol (G-TEP) is an evidence-based form of EMDR. Early evidence from a G-TEP group in THN suggested that the approach showed promise in reducing symptoms of trauma and other mental health disorders. Following the outbreak of the COVID-19 virus and the subsequent government lockdown on 23 March 2020, the whole Service, including the trauma pathway, had to adapt quickly to continue delivering meaningful, high-quality care. EMDR therapists in the Service were trained to use the G-TEP-RISC protocol, which is an adaptation of the G-TEP delivered remotely with, and for, Self-Care. The aim of this reflective piece is to outline adaptations of the THN Trauma Pathway before, and in response to, the COVID-19 pandemic, and our plans for the future.
Introduction
People become traumatised when their ability to respond to a perceived threat is in some way overwhelmed (Levine, 2008). Trauma is associated with disruption and distress, and nationally representative surveys in the USA have suggested that the majority of adults have experienced at least one potentially traumatic event in their lifetime (Kessler et al., 1995; Nickerson et al., 2012). Following exposure to traumatic events, around 25–30 percent of people are estimated to develop Post Traumatic Stress Disorder (PTSD; National Institute for Health and Care Excellence [NICE], 2018) as well as being at increased risk of secondary problems (Shapiro & Laub, 2008).
In 2008 the Department of Health launched the Improving Access to Psychological Therapies (IAPT) initiative as a stepped-care approach to the provision of primary care mental health support. The aim of the IAPT approach was to provide low-intensity treatment for common mental health disorders such as depression and anxiety using cost-effective psychological therapies including Cognitive Behavioural Therapy (CBT), counselling and guided self-help (DOH, 2008).
As recommended by NICE guidelines (2018), both trauma-focused CBT and Eye Movement Desensitisation and Reprocessing (EMDR) are available in IAPT services as treatment options if the individual’s primary presenting problem is related to trauma.
In response to extended waiting lists and the onset of the severe acute respiratory syndrome coronavirus 2 (COVID-19) pandemic we, as an IAPT service in the North East of England, explored the feasibility of adapting our existing EMDR pathways to meet these challenges through group and online delivery methods.
NICE Guidelines
Current NICE guidelines recommend that adults with clinically significant symptoms of PTSD, who have presented to services more than one month after a traumatic event, should be offered an individual trauma-focused CBT intervention (NICE, 2018). EMDR is currently a recommended intervention if these individuals present between one and three months after a non-combat related trauma, with a preference for EMDR if they present more than three months after this event.
Trauma
It is important to consider early intervention when dealing with trauma as individuals who initially cope well at the time of a traumatic event have been known to subsequently develop PTSD (Keller, Burton & Feeny, 2017; Slobodin & de Jong, 2015) as untreated symptoms can become chronic (De Young, Kenardy, Cobham, & Kimble, 2012). Although the majority of people who are exposed to trauma will recover, a large number become affected by clinically significant symptoms for some time afterwards (Shapiro & Laub, 2008). Research has shown that, although the incidence of PTSD symptoms declined in an adult sample following a traumatic event, the natural recovery continued for up to 18 months (Norris et al., 2004), indicating how prolonged this process can be. Even though early access to psychotherapies for PTSD may be beneficial, and EMDR may be a relatively brief treatment (Shapiro & Laliotis, 2015), access to it is frequently limited by extensive waiting list by increasing demand. This presents a challenge for localised services in providing early intervention in the instance of a mass-trauma event.
EMDR
EMDR is a form of psychotherapy which aims to resolve traumatic memories (Shapiro, 2009). Therapeutic change in EMDR is seen as the result of memory reprocessing produced by spontaneously generated internal associations elicited during bilateral stimulation. This method is influenced by The Adaptive Information Processing Model (Shapiro, 2001) which explains trauma (Shapiro, 2014) and other psychiatric disorders (Hase et al., 2017) as the potential result of erroneously stored and integrated representations of stressful events into individuals’ memory networks. Therefore, EMDR, through an eight-phase process (Shapiro & Laliotis, 2015), aims to help individuals to reprocess these stressful events so that they can be fully and adaptively integrated into one’s memory (Ostacoli et al., 2018).
Studies comparing EMDR directly with trauma-focused CBT have shown no significant difference in outcomes, although a trend in favour of EMDR was observed alongside its suggested cost-effectiveness (NICE, 2018; Mavranezouli et al., 2020). Importantly, unlike trauma-focused CBT, EMDR does not require the service-user to provide a detailed description of their trauma, undergo extended exposure to memories, undertake homework, or directly challenge their beliefs (Shapiro & Laliotis, 2015). As a result, it is possible for EMDR to be delivered on consecutive days, giving it an advantage over other therapies in a disaster situation (Shapiro, 2012).
EMDR in IAPT
Within Talking Helps Newcastle (THN)—a primary care mental health service based on the IAPT model—there has been increased demand and subsequent pressure on waiting lists, which echoes the figures demonstrated at a national level. Indeed, referrals to IAPT increased by 11.4 percent from 1.4 million in 2017/18, to 1.6 million in 2018/19 (NHS Digital, 2019).
THN offers EMDR in line with NICE guidelines for trauma. In 2018 it was recognised that the growing demand for one-to-one trauma therapy outstripped the resources that THN could provide across all treatment modalities. To reduce the waiting times for EMDR specifically, an alternative approach was sought.
The R-TEP
In response to the major traumatic incidents of 2017 including the Manchester Arena bombings and Grenfell Tower fire, Elan Shapiro delivered training in the Recent Traumatic Events Protocol (R-TEP) in Manchester and London before coming to the North East and training staff in Newcastle in September 2017 and February 2018.
The R-TEP protocol uses a ‘two-pronged’ approach (past and present) in a one-to-one setting, which enables the episode to cover the consequences of the traumatic event, making it an efficacious EMDR modification for recent events. Following this training—and due to the existing demand for treatment and waiting list already stated—it became apparent that delivering the R-TEP for trauma as a NICE-recommended early intervention within existing IAPT treatment pathways would be challenging.
After attending Shapiro’s training, and with these difficulties in mind, Ericka Johanson (EMDR Consultant at THN) proposed that early intervention could instead be delivered through the Group Traumatic Episode Protocol (G-TEP), which was still in line with NICE guidelines.
The Group Traumatic Episode Protocol (G-TEP)
The G-TEP is a group protocol, modified from the one-to-one R-TEP (Shapiro & Laub, 2008) and has been developed for use with groups of adults, adolescents and children who have undergone a recent traumatic experience or life-changing event with ongoing consequences. Specifically, it has been used following terrorist attacks in Belgium, France, Great Britain, Turkey, and in various disaster zones across the world (Roberts, 2018). Recent ongoing research has also suggested benefit of this treatment for other groups who have experienced potentially traumatic events including refugees (Lehnung et al., 2017) and cancer survivors (Roberts, 2018).
The G-TEP has similarities to the Integrative Group Treatment Protocol (Jarero, Artigas, & Hartung, 2006) which has been recognised as beneficial within disaster situations, although there are also important differences between the two. For instance, the G-TEP protocol centres on a worksheet which encourages deeper processing of trauma memories within a standardised spatial set-up to minimise risks—including dissociation—within the group. Moreover, Section 1 of the worksheet also provides an in-built safety screening tool for inclusion into the group, to highlight individuals who are not yet ready to process their trauma in a group setting. The G-TEP EMDR intervention typically also has smaller group sizes than the Integrative Group Treatment Protocol (Shapiro, 2016).
Group therapy has been shown to be an effective alternative to individual therapy for a range of disorders (Bastien et al.., 2004; Brown et al., 2011). Despite this, service-users often express a preference for individual therapy (Kracen et al., 2013) and a fear of self-disclosure has been identified as one of the key barriers to group therapy engagement (Shchetman & Kiezel, 2016). Unlike most other group interventions, the G-TEP does not require the participants to share the details of their situation with other members. It is hoped that this may begin to break down some of the barriers identified and encourage engagement.
By following the G-TEP, we at THN hoped to reduce traumatic stress, promote adaptive processing, strengthen resilience, and prevent complications arising from trauma for our service-users (Fig 1).
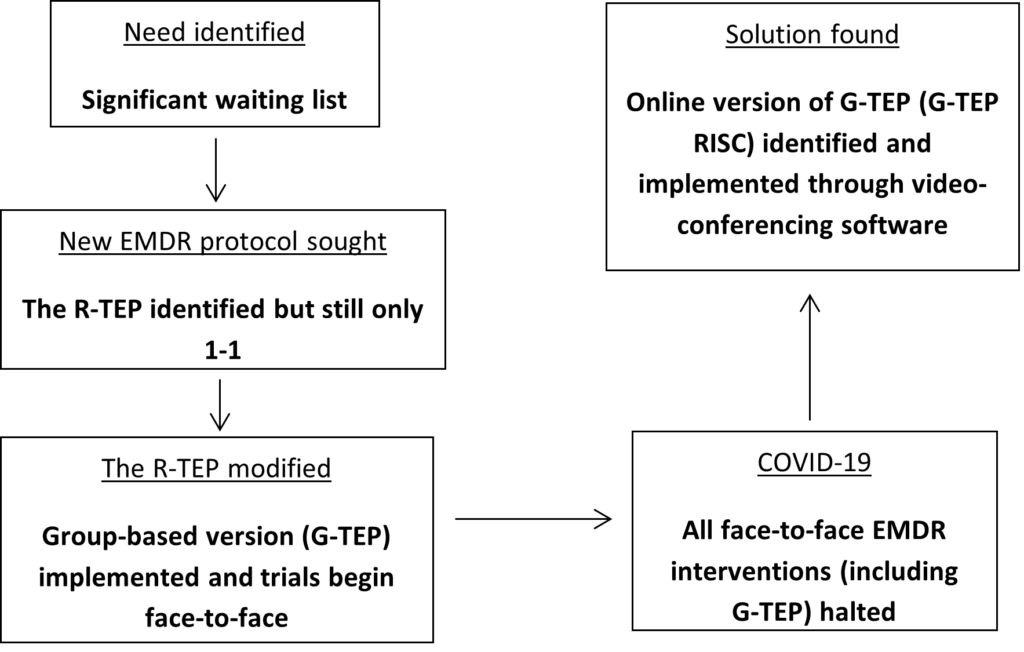
Fig 1: The origins of the G-TEP groups and the G-TEP-RISC in the service, based on an identified need
Method
Following the training in 2017 and 2018, a G-TEP pilot was launched which ran six groups between July 2018 and February 2020. The first groups in July 2018, September 2018, and January 2019 ran as pilot groups and then at least one group every two months were run in November 2019, December 2019, and February 2020 (Fig 2).
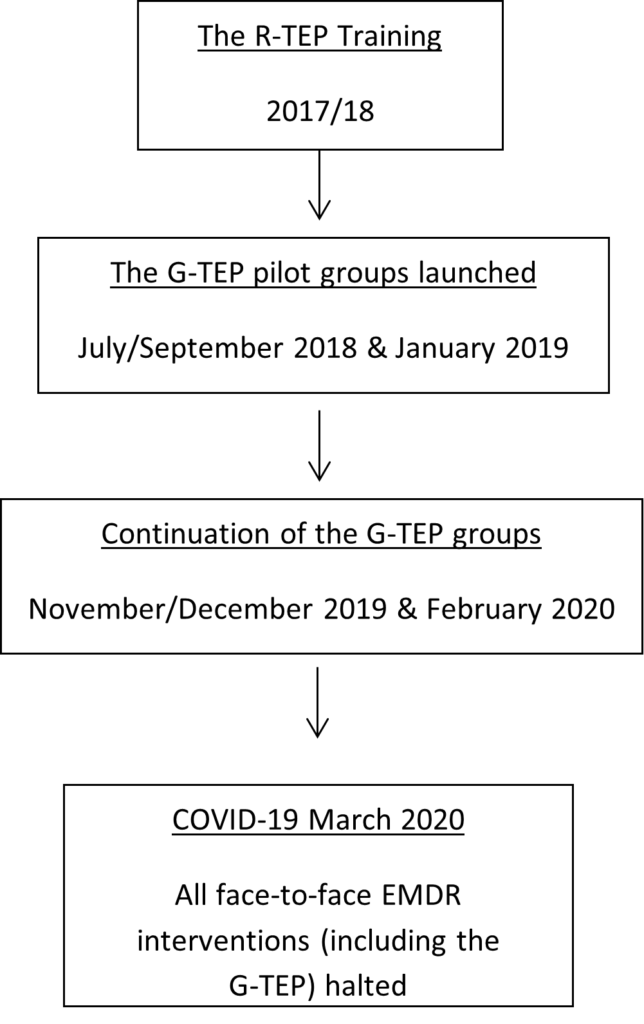
Fig 2: Timeline for the project to date (as halted by COVID-19)
Service-users were recruited into the G-TEP group through the standard service assessment process (Fig 3). Following a telephone assessment, the assessor offered a choice of therapies, of which the G-TEP group was included if appropriate. If the individual selected this option, they were invited to meet with one of the EMDR therapists leading the G-TEP group for an intake interview to ascertain that this treatment was suitable for them. This involved discussing, one-to-one, the traumatic event that they wanted to process and collecting psychometric data. If it seemed that the group would benefit the service-user, a further individual session with the therapist was arranged in order to prepare them for the group. This session involved learning soothing exercises such as ‘Safe Place’ (Shapiro, 2001) and ‘4 Elements’ (Shapiro & Laub, 2008).
The next appointment for all service-users was the group session. This involved groups of up to eight service-users seated around a table, who may have been exposed to the same, or different, critical incidents. Each individual would have a G-TEP worksheet as well as coloured pencils and a sticker. Protocol from the G-TEP Manual 4th Edition was used for these sessions (Shapiro & Moench, 2017).
Groups were facilitated by an EMDR-accredited therapist with significant knowledge of the G-TEP alongside other mental health therapists who were not necessarily trained in EMDR. This worked well as the role of the co-facilitators was to manage distress and assist the service-users with the method.
The intention was to continue with this protocol and evaluate the G-TEP group as a potential improvement to the existing trauma pathway in the service.
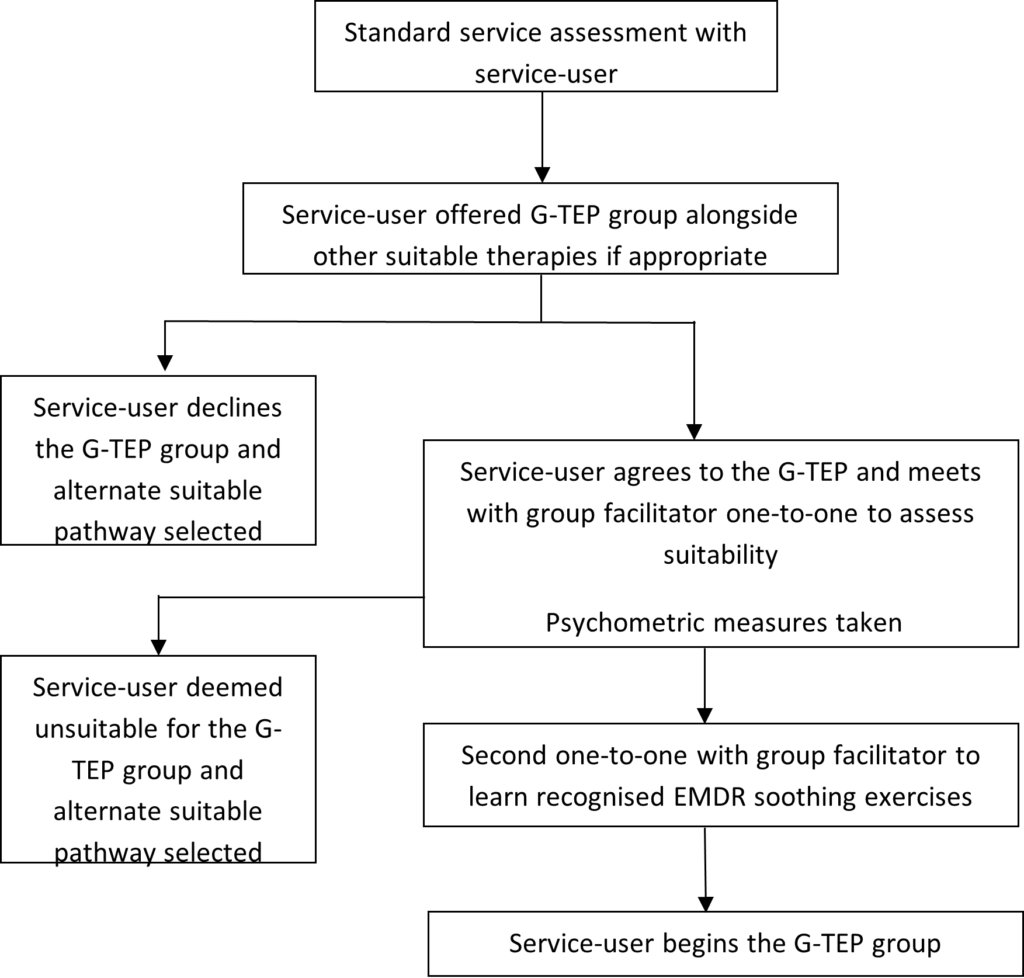
Fig 3: Recruitment process into the G-TEP group
Value of adapting this pathway within the context of COVID-19
In early 2020, we were faced with the unanticipated challenge and disruption of the COVID-19 pandemic. It soon became apparent we would have to again make adaptations to deliver high-quality care in response to this outbreak.
Following government guidance on 23 March 2020, all face-to-face work with service-users at THN (including group work) ceased. All work became remote and therapists were largely offering telephone-only consultations, initially without access to any online platforms. This was a new challenge for many therapists in the service, including EMDR practitioners who previously relied solely on face-to-face sessions.
EMDR Europe (EMDR Europe, 2020) advised that EMDR should not be provided over the telephone and therefore this pathway was temporarily suspended at THN. Those who were waiting for EMDR were transferred to the lengthy CBT waiting list with a view to being offered trauma-focused CBT when they reached the top of the list.
We therefore found ourselves once again unable to offer an early trauma intervention recommended in NICE guidelines (2018) despite the progress we had made. Prior to the COVID-19 lockdown in March 2020, the G-TEP protocol was working well and was producing good results within the service as an alternative to one-to-one EMDR. Initially, the suspension of this pathway caused frustration. However, attention soon turned to how the existing treatment pathway could be further adapted again, but this time in response to the emerging pandemic.
Group Traumatic Episode Protocol for use Remotely with Individuals and for Self-Care (G-TEP RISC)
As it became clear that the ongoing pandemic would prevent a return to face-to-face treatment for considerable time, staff at THN began training in how to work safely online. The EMDR Association of UK and Ireland also then recommended online EMDR. However, this was not recommended by IAPT, and a suitable service-user-facing video conferencing software was not available within our trust at the time. This was resolved within a few weeks, by which time Elan Shapiro had adapted the group protocol worksheet so that it could be used online. This updated protocol was named the G-TEP-RISC (Group Traumatic Events Protocol for use Remotely with Individuals and for Self-Care) and allowed for one-to-one EMDR to be conducted remotely.
Despite the fact that EMDR is a recommended therapy within the NICE Guidance, its online delivery was previously unfamiliar to the service. Therefore, it was decided that the G-TEP-RISC would initially be offered only to a small group of service-users, and evaluated before rolling out to the wider service-user body.
There is currently limited research available on the effectiveness of online EMDR in comparison to in-person delivery. From these limited studies there is a suggestion that there are no differences in patient outcomes (Luber, 2020). Any risks identified with remote delivery are the same as those associated with face-to-face delivery (Luber, 2020). The G-TEP-RISC has therefore been identified as a potential way to safely deliver EMDR remotely.
Although the long-term impact of the global pandemic is yet to be determined, anticipated consequences include trauma following bereavement (Zisook, Chentsova-Dutton, & Shuchter, 1998), social isolation (Vlachos, Papageorgiou, & Margariti, 2020), and frontline healthcare staff bearing witness to death and experiencing extreme levels of stress (Maunder, 2004; Trumello et al., 2020). It is likely therefore that within THN there will be an increased demand for trauma-focused work which we will struggle to meet within a timely manner as recommended by NICE guidelines. The G-TEP-RISC provides an innovative method to continue delivering an early intervention whilst navigating this global pandemic and the changing demands that we expect to see.
Current Findings
Within the past two years, we have adapted the EMDR trauma pathway at THN in response to two very different challenges: reducing waiting times and adapting trauma treatment pathways. Although the G-TEP groups are not currently being offered, the preliminary evidence for those who completed the G-TEP intervention suggests that it is a promising treatment option within a resource-limited IAPT service.
Our early data from the G-TEP group suggests an improvement in symptoms of trauma and other common mental health disorders such as depression and anxiety. These improvements in outcome measure scores appear to also be maintained at one-month post-group, thus indicating the potential longevity of group benefit for service-users as well as the possible utility of this group within other IAPT services who we also encourage to explore this treatment option further. We hope to publish this data in a future publication once the groups can resume.
As more is learned about COVID-19, the utilisation of the G-TEP-RISC as a novel protocol will be evaluated within Talking Helps Newcastle. We hope that, through publication, the G-TEP-RISC will not only become a standardised treatment within our service but that the trauma pathway will continue to be developed. It is our hope that this will improve the service-user experience even when faced with a global pandemic.
References
Bastien, C. H., Morin, C. M., Ouellet, M. C., Blais, F. C., & Bouchard, S. (2004). Cognitive-behavioral therapy for insomnia: comparison of individual therapy, group therapy, and telephone consultations. Journal of consulting and clinical psychology, 72(4), 653-659.
Brown, J. S., Sellwood, K., Beecham, J. K., Slade, M., Andiappan, M., Landau, S., Johnson, T & Smith, R. (2011). Outcome, costs and patient engagement for group and individual CBT for depression: a naturalistic clinical study. Behavioural and Cognitive Psychotherapy, 39(3), 355-358.
Community and Mental Health team, NHS Digital, (2019, July 11) Psychological Therapies, Annual report on the use of IAPT services 2018-19. Retrieved July 31, 2020 from: https://digital.nhs.uk/data-and-information/publications/statistical/psychological-therapies-annual-reports-on-the-use-of-iapt-services/annual-report-2018-19
Department of Health (DOH). (2008) Improving Access to Psychological Therapies Implementation Plan: National guidelines for regional delivery. Crown Copyright: London.
De Young, A. C., Kenardy, J. A., Cobham, V. E., & Kimble, R. (2012). Prevalence, comorbidity and course of trauma reactions in young burn-injured children. Journal of Child Psychology and Psychiatry, 53(1), 56–63.
EMDR Europe (2020) National and International Guidelines. Retrieved 19 August 2020 from: https://emdr-europe.org/research/national-international-guidelines/
Hase, M., Balmaceda, U. M., Ostacoli, L., Liebermann, P., and Hofmann, A. (2017). The AIP model of EMDR therapy and pathogenic memories. Front. Psychol. 8:1578. doi: 10.3389/fpsyg.2017.01578
Jarero, I., Artigas, L., & Hartung, J. (2006). EMDR integrative group treatment protocol: A postdisaster trauma intervention for children and adults. Traumatology, 12(2), 121-129.
Keller, M. S., Burton, M., & Feeny, N. C. (2017). Posttraumatic Stress Disorder. Flessner, C. A., & Piacentini, J. C. (Eds.). Clinical handbook of psychological disorders in children and adolescents: A step-by-step treatment manual. 240-272. Guilford Publications.
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of general psychiatry, 52(12), 1048-1060.
Kracen, A. C., Mastnak, J. M., Loaiza, K. A., & Matthieu, M. M. (2013). Group therapy among OEF/OIF veterans: treatment barriers and preferences. Military medicine, 178(1), 146-149.
Lehnung, M., Shapiro, E., Schreiber, M., & Hofmann, A. (2017). Evaluating the EMDR Group traumatic episode protocol with refugees: A field study. Journal of EMDR Practice and Research, 11(3), 129-138.
Levine, P. A. (2008). Healing trauma: A Pioneering Programme for Restoring the Wisdom of Your Body. Sounds True Inc.
Luber, M. (2020) EMDR Resources in the era of COVID-19 [PDF file] Retrieved 23 October 2020 from: https://marilynluber.files.wordpress.com/2020/06/emdr-resources-for-covid.pdf
Maunder, R. (2004). The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences, 359(1447), 1117-1125.
Mavranezouli, I., Megnin-Viggars, O., Grey, N., Bhutani, G., Leach, J., Daly, C, Dias S, Welton NJ, Katona C, El-Leithy S,& Greenberg, N. (2020). Cost-effectiveness of psychological treatments for post-traumatic stress disorder in adults. PLoS One, 15(4), e0232245.
National Institute for Health and Care Excellence. (2018). Management of PTSD in Children, Young People and Adults (NICE Guideline No. NG116 ). Retrieved 23 July 2020 from: https://www.nice.org.uk/guidance/ng116/chapter/Recommendations#management-of-ptsd-in-children-young-people-and-adults
Nickerson, A., Aderka, I. M., Bryant, R. A., & Hofmann, S. G. (2012). The relationship between childhood exposure to trauma and intermittent explosive disorder. Psychiatry Research, 197(1-2), 128-134.
Norris, F. H., Murphy, A. D., Baker, C. K., & Perilla, J. L. (2004). Postdisaster PTSD over four waves of a panel study of Mexico’s 1999 flood. Journal of Traumatic Stress, 17(4), 283-292.
Ostacoli, L., Carletto, S., Cavallo, M., Baldomir-Gago, P., Di Lorenzo, G., Fernandez, I., … & Oliva, F. (2018). Comparison of eye movement desensitization reprocessing and cognitive behavioural therapy as adjunctive treatments for recurrent depression: The European Depression EMDR Network (EDEN) randomized controlled trial. Frontiers in psychology, 9, 74. doi: 10.3389/fpsyg.2018.00074
Roberts, A. K. P. (2018). The effects of the EMDR Group Traumatic Episode Protocol with cancer survivors. Journal of EMDR Practice and Research, 12(3), 105-117.
Shapiro, E., (2016). Making EMDR more widely available for Early Intervention in Emergency Situations. Retrieved 23 October 2020 from: http://www2.masterapp2.nl/assets/uploads/uploads/21348-den-Hague-2016-PartB.pdf
Shapiro, E. (2009). EMDR treatment of recent trauma. Journal of EMDR Practice and Research, 3(3), 141-151.
Shapiro, E. (2012). EMDR and early psychological intervention following trauma. European Review of Applied Psychology, 62(4), 241-251.
Shapiro, E., & Laub, B. (2008). Early EMDR intervention (EEI): A summary, a theoretical model, and the recent traumatic episode protocol (R-TEP). Journal of EMDR Practice and Research, 2(2), 79-96.
Shapiro, E., & Moench, J. (2017) EMDR Group- Traumatic Episode Protocol (G-TEP) Manual 7th Edition. Retrieved 27 October 2020 from: http://emdrresearchfoundation.org/toolkit/gtep.pdf
Shapiro, F. (2001). Eye Movement Desensitization and Reprocessing (EMDR): Basic Principles, Protocols, and Procedures, 2nd Edn. New York, NY: Guilford Press.
Shapiro, F. (2014). The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: addressing the psychological and physical symptoms stemming from adverse life experiences. Perm. J. 18, 71–77. doi: 10.7812/TPP/13-098
Shapiro, F., & Laliotis, D. (2015). EMDR therapy for trauma-related disorders. In Evidence based treatments for trauma-related psychological disorders, 205-228.
Shechtman, Z., & Kiezel, A. (2016). Why do people prefer individual therapy over group therapy? International Journal of Group Psychotherapy, 66(4), 571-591.
Slobodin, O., de Jong, J. T. (2015). Mental health interventions for traumatized asylum seekers and refugees: what do we know about their efficacy? Int. J. Soc. Psychiatry 61, 17–26. doi: 10.1177/0020764014535752
Trumello, C., Bramanti, S. M., Ballarotto, G., Candelori, C., Cerniglia, L., Cimino, S., … & Babore, A. (2020). Psychological Adjustment of Healthcare Workers in Italy during the COVID-19 Pandemic: Differences in Stress, Anxiety, Depression, Burnout, Secondary Trauma, and Compassion Satisfaction between Frontline and Non-Frontline Professionals. International Journal of Environmental Research and Public Health, 17(22), 8358.
Vlachos, I. I., Papageorgiou, C., & Margariti, M. (2020). Neurobiological Trajectories Involving Social Isolation in PTSD: A Systematic Review. Brain Sciences, 10(3), 173.
Zisook, S., Chentsova-Dutton, Y., & Shuchter, S. R. (1998). PTSD following bereavement. Annals of clinical psychiatry, 10(4), 157-163.




