Online Treatment of Long Covid: A Case Study
This case study will describe how Eye Movement Desensitization & Reprocessing (EMDR) was applied to a case of Long Covid (LC). In LC, the patient continues to experience COVID-19 symptoms for longer than usual after initially contracting SARS-CoV-2 virus, whether they were hospitalised or not (WHO). The process of an in-depth clinical interview to determine case dynamics, formulation or diagnosis of the real issues, will be described, together with a detailed description of the EMDR Protocol using the Flash Technique (FT). This article will also describe treatment outcomes and follow up. Reflections on the reasons for the success of the intervention, on wider COVID issues, therapist self-care and working online with EMDR will conclude this Case study. (Due to my clinical background, I shall use the word “patient” throughout, in the original Latin meaning of the term “Patiens” which means “One who endures”, which, I feel, honours my patients’ suffering more than the term client).
Introduction
Since COVID-19 first appeared on our shores in March 2020, it is indisputable that it has had a devastating impact on our society, culture and behaviour. A recent MORI poll in the UK found that 23% of the population reported having symptoms of Covid Anxiety Syndrome (CAS) which includes fear of returning to normal life, fear of large gatherings, fear of using public transport, compulsive hygiene habits and frequent symptom checking. In Ireland, the Health Research Board recently reported that the prevalence of Post-Traumatic Stress Disorder (PTSD) among a representative sample of 1,000 adults had increased by up to 20% in May 2020.
The Centre for Disease Control (CDC) in Atlanta, USA, suggests that a variety of symptoms occur in LC including: fatigue, shortness of breath, cough, joint pain, chest pain. Other symptoms may also be present including “brain fog”, depression, muscle pain, headache, fever, heart palpitation, rashes, problems with smell and taste, sleep difficulties and memory and concentration difficulties, anxiety and mood changes. As will be shown below, the patient in this study displayed many of the above symptoms when I interviewed her.
Our response to COVID-19 has resulted in multiple losses for our society/culture which may include survivor guilt in relation to colleagues/friends who may have died, or having a safe job working from home when others are in danger; guilt about infecting a loved one; moral injury – being involved in withholding treatment that could save a life; loss of social contact during lockdowns; the effects of social isolation on mental health; “social contagion” of the fear response together with the effects that prolonged fear has on suppressing the immune response, and that has been well documented.
Solomon (2021) refers to the ”loss of our assumptive world” (Janoff-Bulman, 1992), which can trigger earlier trauma that can then interfere with the process of grief and mourning. All of which can leave us struggling with meaning and perhaps becoming obsessed with causality and “survivor guilt”. As one patient said to me recently – “My problems are privileged given what is going on in the world right now”.
I was contacted by this patient via email through my website in September 2020. A psychologist friend in the UK had suggested that she seek EMDR therapy for her symptoms. I followed up with a phone call to her to discuss her needs and to see whether EMDR might have something to offer her, and I concluded it would.
I arranged to conduct an in-depth clinical interview with her online using Skype platform (this was before acquiring familiarity with Zoom) as face-to-face meetings were restricted by government guidelines on the control of COVID-19 in Ireland at that time. This was the first time I had ever considered conducting any therapy online and, naturally enough, I was somewhat apprehensive about how it might work out but, given the lockdown at the time and the urgent need of this patient for some relief of her symptoms, I decided to jump in at the deep end.
Clinical Interview & Assessment
I shall describe the Clinical Interview (CI) process in depth at this point as it is my normal practice before doing any therapy with patients. In this instance, the CI turned out to be crucial in uncovering multiple previous traumas which the patient had not mentioned in the first phone call or email to me. Her focus for treatment was solely on relief from the anxiety associated with COVID-19 symptoms.
I normally use the Beck Depression Inventory II (BDI-II) for corroborative evidence of any clinical indicators of depression. In this instance, due to my own technical limitations of scanning documents, I did not administer the BDI-II and I relied on her responses to my clinical questions regarding sleep, appetite, weight fluctuations, concentration, memory, energy, mood and anhedonia (loss of pleasure in things) to test for the presence of depression.
Equally, before beginning any EMDR intervention, I always check for trauma symptoms using the Impact of Events Scale Revised (IES-R) to validate the reported clinical symptoms of PTSD. Again, in this instance, due to my own technical limitations mentioned above, no administration of the IES-R took place. Instead, I emailed a copy of the Brewin Trauma Screening Questionnaire to the patient. [This scale is a simple 10-point scale involving yes/no answers to statements such as “feeling upset by reminders of the event” or “bodily reactions when reminded of the event” – This scale has a reliability co-efficient of 0.86. For details of how the scale was constructed please see Brewin (2003)]. She completed this before our first therapy session and returned it to me. Her score on this scale was 7/10. The threshold for a confirmation of the presence of trauma on this scale is 6/10. Thus, it was evident that she was indeed suffering from PTSD using both clinical indicators and a psychometric questionnaire. The clinical indicators of PTSD that I use are: flashbacks, nightmares, re-experiencing phenomena, startle response, intrusive images of the event, avoidance and sense of foreshortened future.
I also used the Adverse Childhood Experiences checklist (ACE). This is a 10-item scale involving yes/no answers to items relating to childhood experiences before the age of 18. Her score on this scale was 0/10 which indicated a childhood free from major adverse experiences or traumas. This impression was supported by her answers to my questions about growing up in her Family of Origin (FOO) which will be elaborated upon below.
I took a detailed family history, medical history (including any pre-existing medical conditions such as Diabetes or Hypothyroidism) and an extended family psychiatric history. I also checked for any medications she was currently using (amitriptyline 10 mg prescribed by her GP in May 2020). I further checked for dissociation symptoms such as depersonalisation, derealisation, time losses or absences, hallucinations and paranoia. She reported none of these symptoms. I also asked about her use of drugs (prescribed or otherwise such as coffee, cigarettes, alcohol) to which she reported only having one cup of coffee per day. I also asked about relationship history and current marital situation, which she described as good. She said that her husband is her “best friend”. Finally, I asked, as is my practice, about self-harm history and suicidal ideation or attempts, none of which she reported.
The final part of my clinical interview involves identifying the patient’s strengths and what resources they have for managing strong affect. In terms of her personal history, she was the youngest of four children whose father was a GP. Her childhood was uneventful with a strict upbringing – “You wouldn’t cross them”. She was not bullied at home or at school and she completed her secondary education up to Leaving Certificate in Ireland. She went to college and studied for a career in a health profession in which capacity she has been working since then. She married at 28 years. She has known her husband from the age of 16.
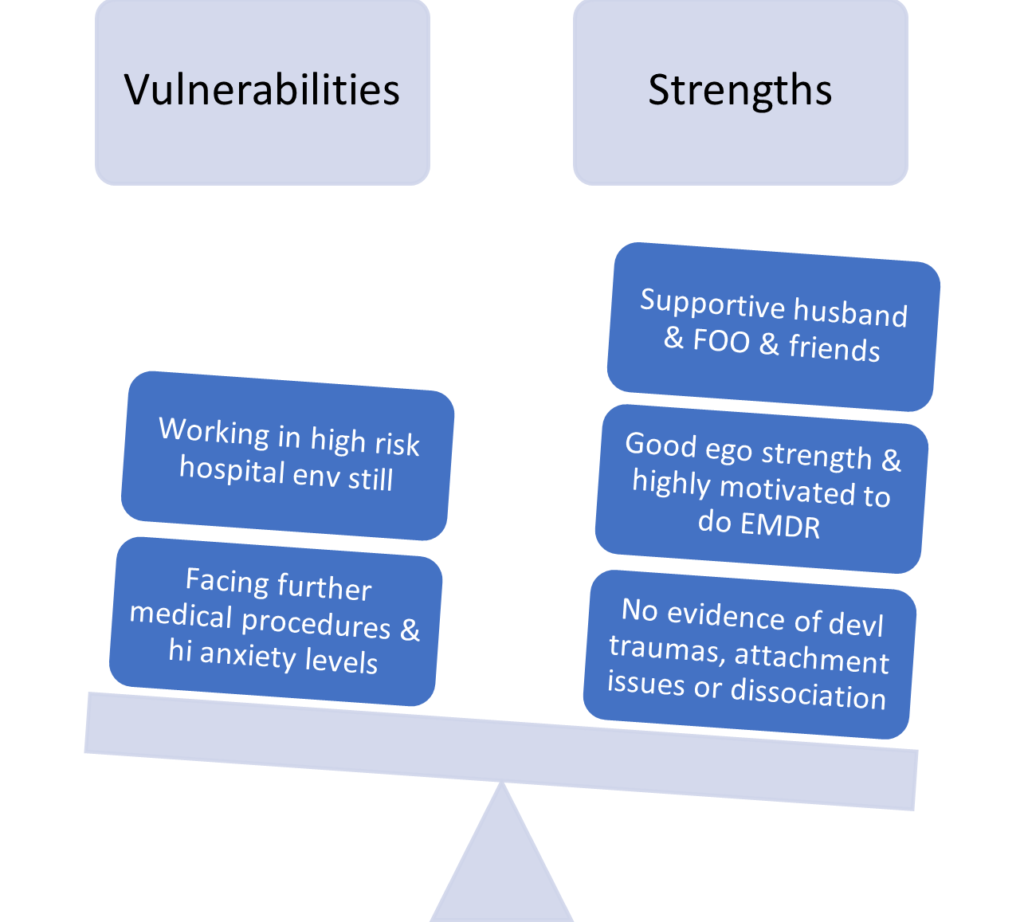
Figure 1: The strengths/vulnerabilities dentified from the clinical interview with this patient
Case History
This patient was a 38-year-old married woman with three sons aged eight,seven and two years old at the time of the clinical interview in September 2020. She was a professional healthcare worker in a large teaching hospital in Dublin. She had contracted COVID-19 in April 2020 and had since been hospitalised twice for tachycardia and persistent fever. Her reported symptoms are outlined in Figure 2 below.
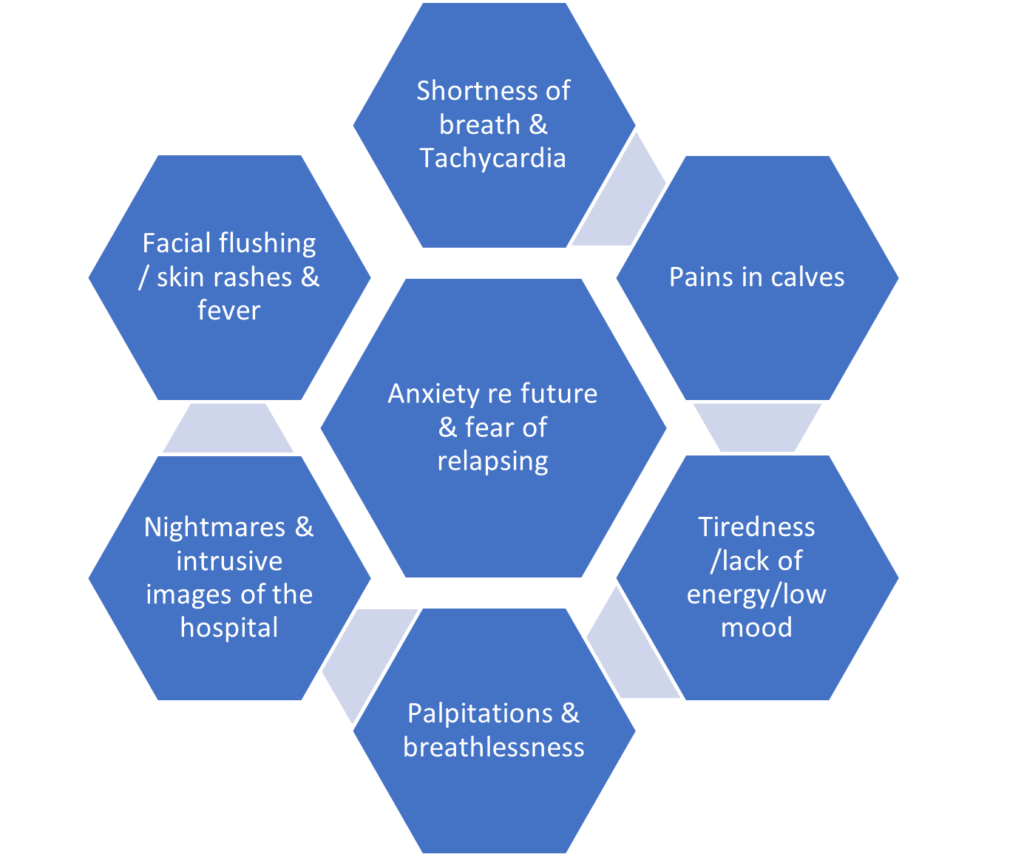
Figure 2: The patient’s reported symptoms
The constellation of symptoms (Figure 2) closely matches the CDC list of symptoms outlined above. In September 2020, the above symptoms were on the wane but she reported increased health-related anxiety, especially with regard to her children and her ability to parent them in the future if she relapsed. To some extent, she was despairing about her future health. She had been taking 10mg amitriptyline since May 2020 with little improvement.
However, she reported many life events, all health related, that had occurred in the previous eight years:
- Eldest son almost died from viral croup in 2012
- She developed “Ocular Migraine” in 2016 which was still present at the time of the interview and associated with her menstrual cycle
- Pregnancy in 2018 with her youngest son was difficult and, at one stage, she had contemplated a termination but delivered herself of “miracle baby” (her words)
- Her mother developed a rare medical condition which involved paralysis on August bank holiday in 2019. It lasted eight months
- Her second son developed febrile convulsions in December 2019 and spent two days in hospital over the holiday period
- Her eldest son contracted Covid in March 2020 and “we nearly lost him” (her words)
- She herself contracted Covid in April 2020 and, prior to September 2020, was hospitalised twice. On one occasion she feared for her life, when her heart rate climbed to 180 per minute
- Her husband contracted Covid in May 2020 and lost his sense of smell
- Her youngest son had diarrhoea for one week in June 2020
It is worth noting that seven of these nine medical incidents occurred in the two years before the clinical interview in September 2020. It was evident that anxiety, depression and PTSD were present and most likely arose from the multiplicity of health-related life events over the past eight years of her life, but especially the seven health emergencies since 2018, less than two years before I saw her. Hence it was not just the presence of LC but also CAS together with a type of medical trauma overload, in my opinion. The seven health emergencies from 2018 to 2020 all involved a near-death experience of a loved one or of her own life. It is widely accepted in the field of trauma that the thought or belief of imminent death is central to the later development of PTSD.
Formulation/Diagnosis
Following from the detailed history taken (above) I used the 5Ps formulation/diagnosis model. See Figure 3 below.
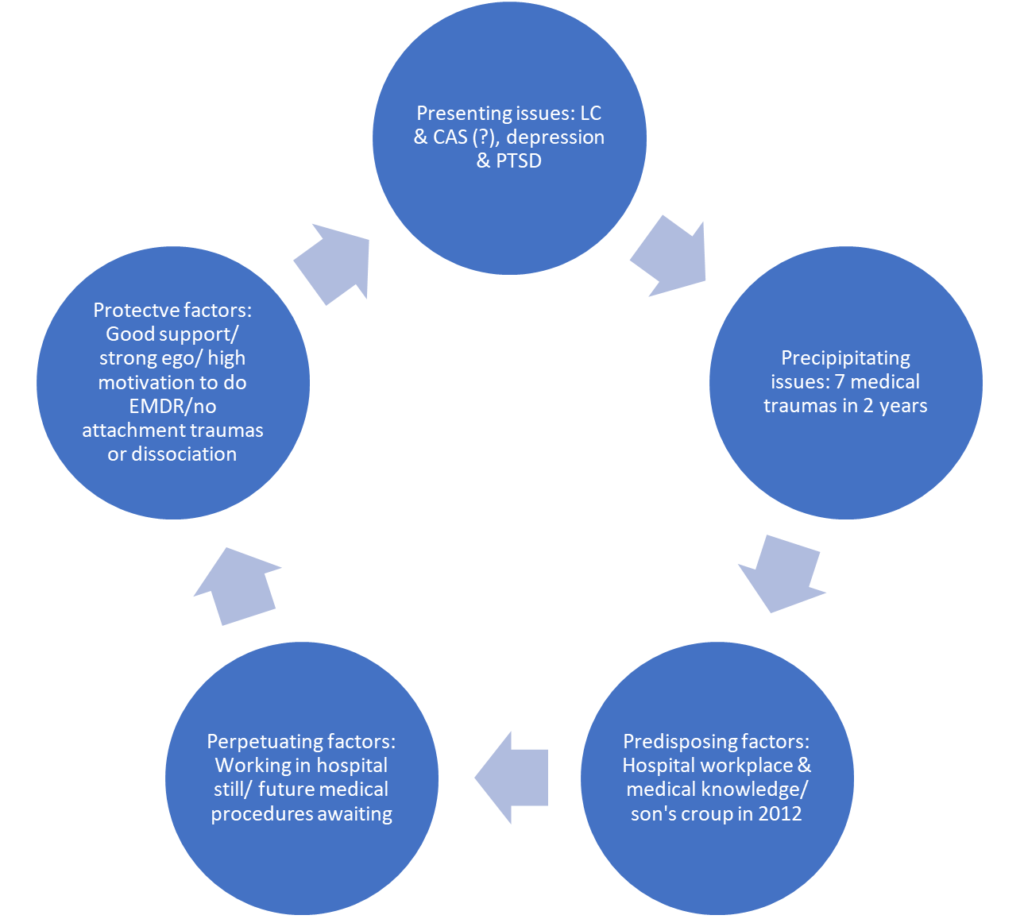
Figure 3: The Five Ps formulation for this patient
The 5 Ps model of diagnosis/formulation helps to identify and clarify the key aspects of the patient’s presentation as well as indicating a pathway to a treatment plan. I cannot emphasise enough how important this approach was with this particular patient; had I just accepted her diagnosis of LC and her anxieties about her future and proceeded to address these issues in therapy, it is highly likely that I would have missed the medical trauma overload over the past eight years of her life and the seven medical incidents between 2018 and 2020. These earlier traumas were key to the development of the treatment plan which we agreed at the end of the clinical interview.
Treatment Plan
The 8 Phase EMDR Standard Protocol formed the basis of the treatment approach. Following the detailed history taking in the clinical interview (Phase 1), the Treatment Plan outlined below was agreed with the patient.
- Resource development
- Address the medical traumas first
- Eldest son’s viral croup 2012
- Pregnancy 2018
- Youngest son’s seizure 2019
- Mother’s illness 2019
- Own Covid experience 2020
- Build future resilience
Phase 2 Preparation: Resource Development
Session 2 began with psychoeducation on the Triune Brain model (MacLean, 1990) in relation to trauma. I have found that when patients develop a good understanding of the Triune Brain model, it often brings a profound sense of relief that the traumatic reactions and somatic sensations which they have been experiencing, are not their fault but arise from the way the brain works. I also explained the concept of the “Window of Tolerance” and taught her some deep breathing. I specifically targeted the “futurising” habit for attention and neutralising as this had developed before therapy began.
“Futurising” is a mental habit of “what if?” thinking where the person imagines the worst possible scenario and then treats that thought as real. A burst of adrenaline usually accompanies such catastrophising and raises the person’s anxiety levels. Interrupting such thinking and bringing oneself back to the present, together with an internal command such as “don’t go there” will usually be enough to neutralise the anxiety cycle. My old Nan used to say “Don’t meet trouble half-way” which is a similar approach.
I also encouraged a more compassionate attitude towards herself with a series of statements such as “I’ve got my L plates up”; “I am surrounded by people who love me” or “I deserve love” which she chose from a list of about 20 such statements. I asked her to copy these statements on to a post-it note and place them at various strategic points in her home (the inside of a cupboard door or on a mirror in the bathroom etc.) or as a screensaver on her computer or wallpaper or mobile phone. The idea being that as she moved about her home during the day, she will read them, and the compassionate statements can begin to become part of her daily life and remind her to move away from self-blame and shame and towards a more self-accepting frame of mind. This was particularly important in this case, as it turns out, which I shall elaborate upon further below in the outcomes and reflections section.
I no longer use the safe place exercise as many patients, especially those with early attachment or developmental trauma, may never have experienced a feeling of safety. Instead, I now use the “oxytocin exercise” (OEx). This exercise involves asking the patient to place a hand on their heart and to think of a memory when they felt very connected to, or close to, another person, or a pet or even a favourite teddy bear from childhood (transitional object) (If the patient has made it to my consulting room, then at some point in their lives, they will have met at least one person with whom they connected). I then ask them to focus on that image of closeness/connectedness. After a few moments, I ask them to notice what they get in their bodies. The vast majority of patients report a warm sensation or feeling of comfort almost anywhere in their bodies. I then explain to them that what has happened, is that they have got a shot of oxytocin just from the memory of feeling close to someone. I explain what oxytocin is – a hormone that is released when we experience a strong bond or closeness with someone such as a mother experiences when breast-feeding her child, or sexual partners have after intercourse, perhaps. I encourage the patient to practice this exercise at least once per day and also explain that it can be used to go to sleep at night or after waking up in the middle of the night. She reacted positively to OEx.
Teaching these six resource exercises to the patient took up all of Session 2. By the end of this session, I felt that she was sufficiently resourced to be able to proceed to processing the traumatic memories of the last two years in the next session.
Phase 3 Assessment: Treatment Goals
Session 3 began with a review of the effectiveness of the coping strategies and resources inculcated in Session 2. She reported success with all of the resource exercises and her motivation was increased to address the various medical traumas that she had experienced over the previous two years.
Various Touchstone Memories (TMs) were identified in agreement with the patient. These included the following images below.
- Eldest son’s croup in 2012 where he was close to death
- Youngest son’s seizure December 2019
- Mother’s illness and paralysis August 2019 – “Thought she would die”
- Her own Covid illness and hospitalization April 2020 – “Thought I was a goner”
- Pregnancy 2018 – Scan @ 16 weeks – two images identified:
(A) “Seeing the obstetrician’s face drop when he saw the scan image” SUDS = 9
(B) Going for a walk during the pregnancy and thinking to herself “He will never hear the birds singing” SUDS = 9
She became extremely distressed when we got to TM5 with both TMs (A & B) as part of the experience of that pregnancy. I decided to process both of these TMs in view of her distress at both poignant images. However, her distress was so great, that I decided to use the Flash Technique (FT) in conjunction with bilateral stimulation (BLS) (Butterfly Hug) . The FT was developed by Manfield, Lovett, Engel and Manfield (2017) and Manfield, Engel, Greenwald and Bullard (2021) for when the SUDS are high or the patient has difficulty facing the memory/images to process overwhelming TMs. [For further information on training in the FT please see www.flashtechnique.com]. The FT has been shown to be effective in reducing the disturbance of TMs in as little as 10 – 15 minutes (Manfield et al., 2017, 2021). That was certainly the case with this patient as her SUDs decreased to zero for both TMs after 15 minutes.
Once the TMs had been processed successfully down to SUDS = 0, I then did closure, grounding and debrief at the end of session 3. She spontaneously said at the end of the session “I’m proud of what I’ve done here today” which I regarded as a positive cognition (PC) which did not require installation.
Phases 4 – 8
Session 4 began with a review of Session 3. No adverse reactions (NAR) were reported by the patient and SUDs were zero for both TMs processed in the previous session.
We agreed to address the trauma of her youngest son’s seizure in December 2019 as this was still very fresh in her mind nine months later. The TM identified was “Him shaking in my arms and I’m on the phone to the services screaming ‘Tell me what to do’”. The SUDs were seven for this image and the negative cognition (NC) was “I’m not in control”. This image was processed using OEx, FT and BLS to SUDS = zero within 5 minutes but four other TMs emerged during this processing which were TM (1) “His little face” in the car on the way to the children’s hospital; TM (2) An argument with the admitting doctor at the door of the hospital who tried to make her leave; TM (3) Aftermath a few days later when her son had a relapse; TM (4) Her other sons’ “little faces” when they witnessed their brother’s seizure. SUDs for all of these TMs ranged from four to seven.
These four TMs were all processed successfully to SUDS = zero after 20 minutes using OEx, FT & BLS. The PC which was agreed with the patient was “I did my best” and whose Validity of Cognition (VoC) rose to seven after 5 min. The session ended with closure, grounding and debrief.
Session 5 began with a review of Session 4. The patient reported NAR following Session 4 and SUDs for all TMs processed in that session remained at zero. We agreed to process the TM of her eldest son’s viral croup in 2012. SUD = nine for this TM then almost eight years later and the NC was “I didn’t act fast enough”.
She reported two separate TMs associated with this traumatic experience which were: TM (1) “Dad’s face when he saw my son” which had a SUD of nine and TM (2) “When my son stopped breathing in the car in heavy traffic on the way to the children’s hospital” which had a SUD of eight. In relation to TM (1), the reader will recall that her father was a GP so his reaction to seeing his grandson had major significance on her. Both TMs were successfully processed to SUD = zero after 20 minutes using OEx, FT and BLS.
However, a new TM emerged thatwas a memory involving the same boy in 2016 when he developed Orbital Cellulitis whilst the family were on holiday in Portugal and his eye “swelled up like a balloon”. The TM here was “Rushing him through the streets in a pram to hospital” which had a SUD of nine. This was processed successfully to SUD = zero within 15 minutes using FT and BLS. The VoC was “I did the best I could” which increased to seven within five minutes. At the end of this session, I did closure, grounding and debrief and before the session ended, she said spontaneously “I can let go of the burden I’ve been carrying all these years”, which I validated.
Session 6 began with a review of Session 5 and its aftermath. She reported feeling drained and “numb” for about 24 hours after Session 5 which then dissipated without any further adverse reactions reported. We agreed to process the TM of her mother’s illness which occurred over the August bank holiday in 2019. She reported two distressing images associated with this trauma which were: TM (1) Conducting a bedside vigil at the hospital which had a SUD of nine and TM (2) In the hospital car park with her father whom she described as “A broken man” which had a SUD of seven.
TM (1) was processed to SUD = zero after 15 minutes using OEx, FT and BLS. TM (2) was similarly processed to SUD = zero after 10 minutes. During the processing of TM (2) a new memory emerged: receiving a phone call from the nursing home where her mother was recuperating. This image had a SUD of seven. This memory was processed to SUD = zero after five minutes using OEx, FT and BLS.
Given the number and complexity of medical trauma memories and images, I adapted the Standard EMDR Protocol for her to run a movie of the whole experience, from bank holiday Monday 2019 to Christmas 2019, when her mother had fully recovered. She recalled more details of her mother’s illness during the running of this movie, but these were not overwhelming for her and represented, I felt, her attempts to integrate and assimilate her mother’s illness into her own historical memory in a way that made sense for her. She spontaneously said at the end of this process “I futurise too much” which I regarded as a PC and on checking with her, the VoC was seven for this insight. The session ended with closure, grounding and debrief as per the EMDR Protocol.
Session 7 began with a review of Session 6. She reported NAR following Session 6. She emphasised the positive impact which the PC “I futurise too much” had on her in the week between Session 6 and Session 7. In this session, we agreed to process her own Covid illness from April 2020.
She identified nighttime in bed, with her heart racing, shortness of breath and her arms feeling numb as her TM. The NC associated with this TM was “I’m going to die” with a SUD of 10. This TM was unusual as there were other NCs associated with the image which included: “I’ll never work again” and “I will never be well again” both of which had SUDs of 10. (I noted at the time that both NCs were a form of futurising but did not share this with the patient at that time).
The TM and all three NCs were processed using OEx, FT and BLS to SUD = zero before the end of the session. During the processing, another TM emerged which was “Saying farewell to my children whilst they slept before I went into hospital” which also had a SUD of 10. This was also processed to SUD = zero before the end of the session. During the processing of this second TM image, further details of her Covid illness were recalled spontaneously which included the hospital staff wearing Hazmat clothing and “being treated like a leper” by hospital staff which were both distressing for her but not overwhelming and were quickly processed also. All of the above TMs were processed to SUD = zero before the session ended 40 minutes later. Closure, grounding and debrief completed the session. She spontaneously commented at the end of the session how she had come to realise “just how much I futurise”, similar to Session 7.
Session 8 began with a review of Session 7 and its aftermath. She reported NAR following the previous EMDR session and SUDs were zero for all the TMs processed in Session 7. A review of all the TMs processed over the previous six sessions revealed that all TMs had SUDs of zero, which was very surprising to me but also very gratifying for her. Loss and anticipatory loss was a major theme which emerged from our review together – loss of good health, loss of parenting, loss of her children’s future, loss of her career together with feelings of shame and guilt over having Covid. Also, she identified just how much she “futurises” in the course of her everyday life and how this kind of thinking raises her anxiety levels, which was a major revelation for her, but perhaps more importantly, what to do about it and how to change it to regulate her anxiety. I also helped her to distinguish between a lapse/ relapse and a collapse after therapy which can help patients put any “slippages” or any re-emergence of “old stuff” patterns into context for themselves, rather than catastrophising and self-blaming post-treatment.
As per the EMDR Protocol and the treatment plan, building resilience was an important aspect of this review session. I did a future template with her six months into the future (April 2021) where she imagined herself fully recovered from Covid and leading a normal life again with her family and at work. We reviewed the key outcomes / recovery experiences which she found helpful in the EMDR approach. These are listed below.
- Live more in the present – “What is, not what if”
- Compassion for herself and what she had been through over the past eight years of her life but especially the seven medical traumas of the last two years, which included LC and how most people would probably feel similarly to her if they had experienced what she had gone through
- Developed a plan to cope – “If X happens then I shall do Y” as opposed to “What if” thinking
- Recognise that anniversary dates and times of the year may “trigger” anxiety reactions or trauma spikes and how to cope with these if they do occur
We agreed that she could contact me as and when she felt she might need to and that I would make contact with her in 6 – 12 months’ time to check on progress. The therapy sessions concluded at this point. All in all, the eight online therapy sessions lasted from early September 2020 to the end of October 2020.
Review of Therapy and Follow-up
In June 2021, I telephoned the patient as agreed and she reported that her overall health was “Excellent”. She had recovered physically and was now free of all the physical symptoms which she had with COVID-19. She was running 5km daily. She had ceased taking amitriptyline in May 2020 without any relapse in functioning. Her sleep pattern had returned to normal. She told me that she can have a glass of wine again now! Her youngest son had come into close contact with another child who had COVID-19 at the childminders and she had coped with that. She had thought she would react with a panic attack but she hadn’t. As she stated “I’m fully functioning again now and I don’t feel that I am being held back”. Her score on the Brewin Trauma Screening Questionnaire was 0 / 10. All of which was good news.
In preparation for this case study, I checked with her again at the beginning of October 2021 – 12 months after therapy ended. She told me that she was back to “Full Life now” and she was working two days per week, teaching Pilates and working in the hospital, which she felt was a good work-life balance for her. She felt that she was better able to regulate her emotions and she no longer “futurised”. She finds the breathing exercise still helpful to her and uses it regularly during the day. There was no evidence of the CAS which she had presented with on assessment.
Interestingly, she reported that she has not had an Ocular Migraine in the last year, since therapy ended, which was a fascinating finding, in my opinion. One of her sons had an allergic reaction in his eye recently and she had coped well with that, which again was evidence of the effectiveness of therapy given the Ocular Cellulitis experience in Portugal five years previously with another of her sons.
She stated that she still thinks about Covid but does not become dysregulated or over-whelmed – it is now part of her history, that is, “Old stuff”! But perhaps the most gratifying finding was the fact that she is now working with her employer (a major teaching hospital) in developing a rehab programme for patients with LC given that she herself is a survivor. As she put it – “I’m proud to be giving something back”. This is a good example of post- traumatic growth, I believe!
Conclusions and Reflections
This case study has described a case of LC presenting co-morbidly with CAS and medical traumas overload in the two years before she became infected with COVID-19. I have described the in-depth clinical assessment process which was crucial in elucidating the co-morbid issues of medical traumas which were not her chief concern when she first contacted me. I have outlined the treatment process using the EMDR Protocol with the FT as a major part of the therapy process, which was very successful at helping her to process many very distressing images and memories of the two years prior to her developing LC. In a 12-month follow-up the gains of EMDR therapy were maintained and she had returned to her pre-LC functioning without any evidence of CAS or raised anxiety levels. There was even evidence of post-traumatic growth as she is participating in developing a rehab programme in her hospital workplace for patients with LC.
The limitations of case studies are well documented. They include the lack of generalisability to the wider population, researcher bias, and atypical presentation of the presenting case . Notwithstanding these limitations, this case study has demonstrated the concept of “model utility”, especially as it relates to conducting EMDR therapy online, as well as showing the effectiveness of FT in resolving extremely distressing memories over the traditional EMDR Protocol in the shorter time scale of eight sessions. This study has also confirmed the long-term effectiveness of online EMDR Therapy in that the gains evidenced at the end of eight therapy sessions were maintained at 12-month follow up when the patient had returned to pre-morbid physical, psychological and emotional well-being. Thus, this case study may be considered to be an example of evidence-based practice in operation.
In reflecting on the overall case, the importance of the in-depth clinical assessment and interview cannot be overstated. Without this part of the EMDR Protocol, it is doubtful as to whether the medical traumas overload in the patient’s history would have been uncovered. Thus, the in-depth clinical assessment was essential to arriving at a comprehensive formulation and sound treatment plan in consultation with the patient.
Regarding the Standard Protocol, the FT proved to be central to the successful outcome of this case study. Manfield et al. (2021) claim that FT is safe, simple, rapid and effective, and can speed up the processing of TMs. As indicated previously, FT was developed to help patients process memories or images that are too painful or distressing to face in the Standard Protocol. It was designed to be used when the SUDs are high or the patient has difficulties facing the memories. That was certainly the case for this patient whose SUDs were often 10, even years after the event. FT was also designed to be a relatively painless method of reducing the intensity of the TMs so that they can be processed and this proved to be the case in this study. I also think that one of the reasons as to why the FT worked so effectively in this case, was the absence of “feeder memories” (Manfield et al., 2021). “Feeder memories” are those memories from an earlier trauma that can arise during therapy and disrupt the FT processing. There were no developmental traumas or early attachment wounds elicited in this patient’s history which was a significant factor in enabling a relatively straightforward therapeutic process to take place and also facilitated swift and effective FT processing.
In terms of working with LC it became apparent very early in the process in this instance, just how important were the pre-morbid experiences this patient had experienced. She had experienced seven medical traumas in the two years prior to contracting COVID-19. Thus, it is highly likely, with this level of stress, that her immune system was sub-optimal by the time she contracted COVID-19. She also worked in a large hospital which was a high-risk environment for getting COVID-19. These factors all contributed, I believe, to the development of LC in her case.
Reflections on Online EMDR
This was my first foray into online therapy and, as such, it was a little daunting. In September 2020, I was still using Skype but have since moved on to conduct therapy sessions on WhatsApp, Zoom and now, Dox.me, which is a dedicated telemedicine platform for health professionals with more secure features than either Zoom or Skype. I think it isimportant when doing therapy online, to have a back-up platform such as WhatsApp which is phone-based in case anything goes wrong, which it can sometimes do due to poor Wi-Fi or sound/vision difficulties arising. Basic video etiquette includes using a quiet room with no background noise such as TV, radio or dogs barking, sitting facing the light source, encouraging the patient to have water and tissues to hand during the session as well as some paper and pen to make notes etc. Clearly it is important to switch off one’s own mobile phone as well as asking the patient to do the same in order to avoid interruptions.
Apart from the technical issues outlined above, online therapy is nonetheless, not the same as sitting face-to-face with the patient. The therapist has much fewer non-verbal cues to work with as one only has the patient’s head and shoulders in the camera range. Nonetheless, strong affect can, and will, be experienced by the patients during EMDR processing online. The same containment and supportive interventions are needed online and can work just as effectively in my experience of online therapy to date. The Standard EMDR Protocol worked well in this online case study, especially using FT, and although the online experience was less “rich” than face-to-face therapy, I would encourage readers to not let the “Best be the enemy of the good” and to give online therapy a go!
Reflections on Therapist Self Care in the time of Covid
The following are a number of suggestions which the reader may hopefully find helpful. In view of the unrelenting negative media coverage of COVID-19 and case numbers since March 2020 (and especially the lack of distinction in the case numbers between dying “from” Covid as opposed to dying “with” Covid), I decided to limit my exposure to news bulletins and reports. I came off all social media and now only buy a weekly magazine which keeps me up to date with developments of the past week. Reading encourages “slow brain” activity (Kahneman, 2012) as opposed to TV, videos, YouTube and social media, which encourage “fast Bbrain” activity. It has been established (Dobelli, 2021) that constant exposure to news media (and social media) has the effect of reinforcing hindsight bias, availability bias, confirmation bias, learned helplessness, passivity, lowering of attention span, concentration and comprehension, as well as re-wiring our brains. Thus, reducing and limiting our exposure to the constant news cycle can help our own emotional regulation and mental well-being.
Reflections on the Wider Effects of Covid
As someone from a Cognitive Behaviour Therapy (CBT) background, I have been struck by how our beliefs/thoughts and cognitions have created the psychological issues for our society in relation to Covid. Epictetus, a Greek Stoic philosopher about 2000 years ago wrote “What disturbs and alarms man (sic) are not the things but his (sic) opinions and fancies about the things”. Shakespeare also said something similar in Hamlet when he had Polonius say “There is nothing either good or bad but thinking makes it so” (Act 2, Sc 2). In more recent times Eric Bogle, an Australian folk singer, who wrote the song “The band played waltzing Matilda” had the immortal line “I never knew there were worse things than dying”.
It is also important to become aware of the role of “safety behaviours” in maintaining fear. afety behaviours are those behaviours that we engage in in the hope of warding off negative consequences such as avoiding stepping on the cracks on the pavement. The injunction to “stay safe” can, unwittingly, increase fear. It is also well established in the literature that prolonged fear compromises the immune system and, counterintuitively, can work against the objective of keeping people safe and healthy in the longer term. There is the distinct possibility that what we have witnessed in our societies since the arrival of Covid is the “nocebo effect”. Most readers will know of the placebo effect in terms of drugs research and how the placebo effect creates a positive response on the basis of the belief the patient has that the medication/tablet/treatment will do them good. The nocebo effect is the converse of this; negative expectations can amplify and create worse effects than the virus might otherwise have had which, I would argue, is what has been widespread in our society, especially in the media coverage of COVID-19.
Finally, beware the “Covid state of mind” (Solomon, 2021). This happened to me recently when a friend of mine told me about a play he attended. I was initially shocked to hear that he had been so brash as to attend a play but did not say anything to him. On arriving home and reflecting on my own reaction, I came to realise that I had internalised the lockdown and was living a version of Solomon’s (2021) “Covid state of mind”. This is not the way to live our lives. As an 80-year-old woman said to me recently “ I want to live till I die”.
References
Brewin, C. (2003). Posttraumatic stress disorder: Malady or myth. Yale: UP.
Dobelli, R. (2020). Stop reading the news.London: Sceptre books.
Janoff-Bulman, R. (1992). Shattered assumptions: Towards a new psychology of trauma”. NY: Free Press.
Kahneman, D. (2012). Thinking fast, thinking slow. London: Penguin Books.
MacLean, P. (1990). The triune brain in evolution, NY: Springer.
Manfield, P. E., Lovett, J., Engel, L., & Manfield, D. (2017). Use of the flash technique in EMDR therapy: Four case examples. Journal of EMDR Practice & Research, 11 (4), 195-205.
Manfield, P. E., Engel, L., Greenwald, R., & Bullard, D. G. (2021), Flash technique in a scaleable low-intensity group intervention for COVID-19 related stress in healthcare providers. Journal of EMDR Practice & Research,15 (2).
Solomon, R. (2021). https://etq.emdrassociation.org.uk/2021/03/27/how-covid-further-complicates-grief
WHO/2019-nCoV/Post_COVID-19_condition/Clinical_case_definition/2021.1




